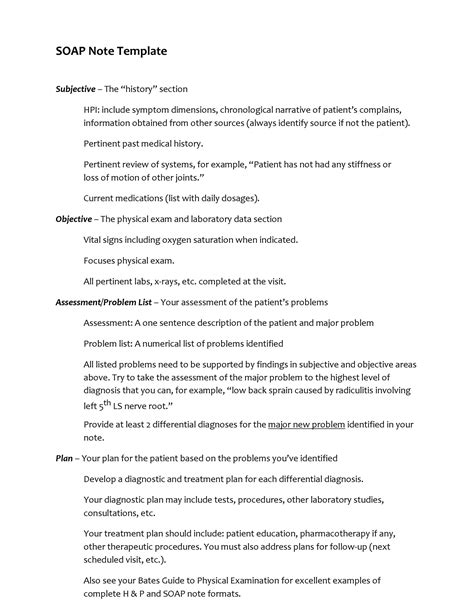
Soap notes are a crucial documentation tool in healthcare, providing a standardized method for recording patient information, treatment plans, and progress. Developed by Dr. Lawrence Weed in the 1960s, the SOAP note format has become a widely accepted and essential component of medical documentation. The acronym SOAP stands for Subjective, Objective, Assessment, and Plan, each section serving a distinct purpose in the patient care process.
Understanding the SOAP Note Format
The SOAP note format is designed to ensure that healthcare providers document patient information in a clear, concise, and organized manner. This format not only facilitates effective communication among healthcare team members but also helps in tracking patient progress over time. Below is a detailed explanation of each component of the SOAP note, along with examples to illustrate their application in real-world scenarios.
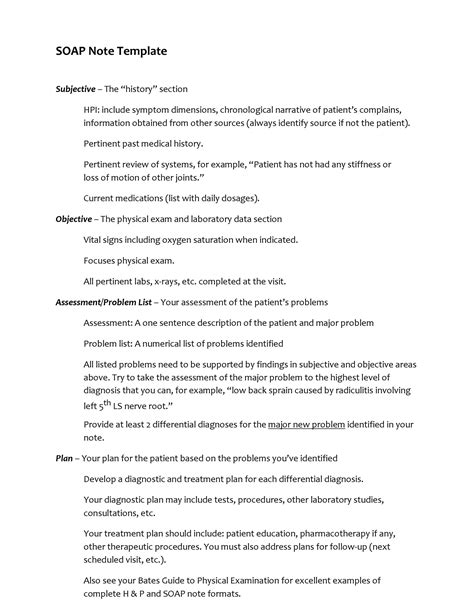
Subjective (S) Section
The Subjective section of the SOAP note includes information provided by the patient, such as their symptoms, medical history, and any concerns they may have. This section is crucial as it offers insight into the patient’s experience and perspective on their condition. For instance, a patient might report experiencing chest pain, difficulty breathing, or recent changes in their appetite or sleep patterns.
| Category | Example |
|---|---|
| Patient's Chief Complaint | "I've been having severe headaches for the past week." |
| Medical History | "I have a history of hypertension and am currently taking medication for it." |
| Current Symptoms | "I've noticed swelling in my legs and feet over the past few days." |
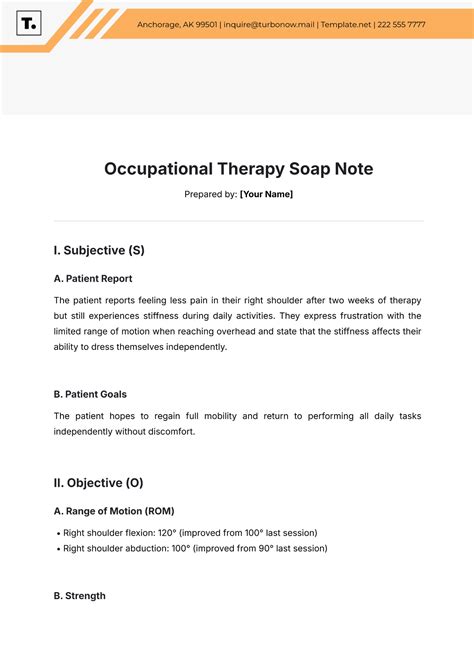
Objective (O) Section
The Objective section contains measurable, observable data collected by the healthcare provider during the patient’s visit. This can include vital signs, laboratory results, physical examination findings, and other diagnostic test results. For example, a patient’s vital signs might show an elevated blood pressure of 140⁄90 mmHg, or laboratory results might indicate an increased white blood cell count suggestive of an infection.
| Category | Example |
|---|---|
| Vital Signs | Blood Pressure: 140/90 mmHg, Heart Rate: 88 bpm |
| Physical Examination Findings | "Tenderness noted in the abdominal region upon palpation." |
| Laboratory Results | White Blood Cell Count: 15,000 cells/μL (elevated) |
Assessment (A) Section
The Assessment section involves the healthcare provider’s diagnosis or impression of the patient’s condition based on the information gathered in the Subjective and Objective sections. This is where the provider synthesizes the data to determine the underlying cause of the patient’s symptoms. For instance, a patient presenting with symptoms of fever, cough, and shortness of breath might be assessed as having pneumonia.
Plan (P) Section
The Plan section outlines the treatment strategy, including any medications prescribed, lifestyle changes recommended, further diagnostic tests needed, and follow-up appointments. This section is critical for ensuring that the patient receives appropriate care and for monitoring their response to the treatment plan. For example, a patient diagnosed with hypertension might be prescribed an antihypertensive medication, advised to reduce sodium intake, and scheduled for a follow-up visit to assess the effectiveness of the treatment plan.
| Category | Example |
|---|---|
| Medications | Prescribed Amlodipine 5mg once daily for blood pressure management. |
| Lifestyle Modifications | Recommended a low-sodium diet and regular physical activity. |
| Follow-Up | Scheduled a follow-up appointment in 2 weeks to monitor blood pressure. |
Key Points
- The SOAP note format is a standardized method for documenting patient information, facilitating clear communication among healthcare providers.
- The Subjective section includes patient-reported information, such as symptoms and medical history.
- The Objective section contains measurable data, including vital signs and laboratory results.
- The Assessment section involves the healthcare provider's diagnosis based on the collected data.
- The Plan section outlines the treatment strategy, including medications, lifestyle changes, and follow-up appointments.
Effective use of the SOAP note format is critical for providing high-quality patient care. By ensuring that all components of the SOAP note are thoroughly completed, healthcare providers can develop comprehensive treatment plans, track patient progress, and make informed decisions regarding patient care.
What is the primary purpose of the SOAP note format in healthcare?
+The primary purpose of the SOAP note format is to provide a standardized method for documenting patient information, ensuring clear and effective communication among healthcare providers and facilitating high-quality patient care.
How does the SOAP note format contribute to patient safety?
+The SOAP note format contributes to patient safety by ensuring that all relevant patient information is documented and communicated clearly among healthcare providers, reducing the risk of errors and adverse events.
Can the SOAP note format be used in all healthcare settings?
+Yes, the SOAP note format can be used in all healthcare settings, including hospitals, clinics, and private practices, as it provides a universal language for documenting patient care.
In conclusion, the SOAP note format is a vital tool in healthcare, offering a structured approach to patient documentation and care planning. By understanding and effectively utilizing the SOAP note format, healthcare providers can enhance patient outcomes, improve communication among the healthcare team, and contribute to the overall quality of care provided.