The Joint National Committee 8 (JNC 8) guidelines, published in 2014, mark a significant shift in the approach to managing hypertension in adults. These guidelines, developed by a panel of experts appointed by the National Heart, Lung, and Blood Institute (NHLBI), aim to provide evidence-based recommendations for the diagnosis, evaluation, and treatment of high blood pressure. A critical aspect of the JNC 8 guidelines is their emphasis on individualizing care, considering factors such as the patient's age, the presence of comorbid conditions like diabetes or chronic kidney disease, and the potential risks and benefits of various treatment strategies.
Key Components of the JNC 8 Guidelines

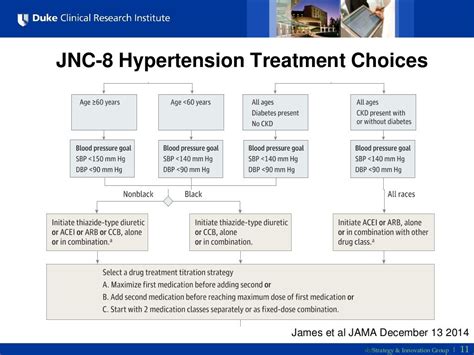
The JNC 8 guidelines introduce several key components that differentiate them from their predecessors. One of the most notable changes is the recommended blood pressure targets for different patient populations. For individuals aged 60 years and older, the guidelines suggest a target systolic blood pressure of less than 150 mmHg, while for those younger than 60 years, the target is less than 140 mmHg. Furthermore, for patients with diabetes or chronic kidney disease, the recommended target is also less than 140 mmHg. These recommendations are based on a thorough review of clinical trial data, indicating that these targets can help minimize the risk of cardiovascular events without significantly increasing the risk of adverse effects.
Pharmacological Treatment
The guidelines also provide recommendations for the initial pharmacological treatment of hypertension. They suggest that the choice of initial therapy should be based on the presence of specific comorbid conditions. For example, in patients with chronic kidney disease, an angiotensin-converting enzyme inhibitor (ACEI) or an angiotensin receptor blocker (ARB) is recommended as initial therapy due to their renoprotective effects. Similarly, for patients with heart failure, an ACEI or ARB, possibly combined with a beta-blocker, is considered optimal. The guidelines emphasize the importance of using the lowest effective dose of medication and gradually increasing it until the blood pressure target is achieved or the maximum tolerated dose is reached.
| Condition | Recommended Initial Therapy |
|---|---|
| General Population without CKD or Diabetes | ACEI, ARB, CCB, or Tiazide-type diuretic |
| CKD | ACEI or ARB |
| Diabetes | ACEI or ARB |
| Heart Failure | ACEI or ARB + Beta-blocker |
Implications and Controversies
The publication of the JNC 8 guidelines has been followed by both praise and criticism. Some have welcomed the simplified approach to blood pressure management, while others have expressed concerns about the potential for undertreatment, particularly in younger patients or those with higher cardiovascular risk. The debate surrounding the guidelines underscores the complexity of hypertension management and the need for continuous research and evidence-based practice.
Lifestyle Modifications
In addition to pharmacological interventions, the JNC 8 guidelines emphasize the importance of lifestyle modifications in the management of hypertension. These include dietary changes such as the DASH (Dietary Approaches to Stop Hypertension) diet, increased physical activity, weight loss for those who are overweight or obese, and reduction in alcohol consumption. The guidelines acknowledge that while these modifications can be effective in lowering blood pressure, they may not be sufficient for all patients, and pharmacological treatment may also be necessary.
Key Points
- The JNC 8 guidelines recommend individualized blood pressure targets based on age and comorbid conditions.
- The choice of initial pharmacological therapy should consider the presence of specific comorbid conditions.
- Lifestyle modifications are a critical component of hypertension management.
- The guidelines aim to balance the benefits of blood pressure reduction with the potential risks of treatment.
- Continuous monitoring and adjustment of treatment are necessary to achieve and maintain optimal blood pressure control.
In conclusion, the JNC 8 guidelines represent a significant advancement in the management of hypertension, emphasizing a patient-centered approach and the importance of evidence-based practice. While debates and controversies surrounding the guidelines exist, they provide a foundational framework for healthcare providers to tailor treatment strategies to the unique needs and circumstances of each patient, ultimately aiming to reduce the burden of cardiovascular disease.
What are the main recommendations of the JNC 8 guidelines for blood pressure targets?
+The JNC 8 guidelines recommend a blood pressure target of less than 150⁄90 mmHg for individuals aged 60 years and older, and less than 140⁄90 mmHg for those younger than 60 years, as well as for patients with diabetes or chronic kidney disease.
How do the JNC 8 guidelines approach the choice of initial pharmacological therapy for hypertension?
+The guidelines suggest that the choice of initial pharmacological therapy should be based on the presence of specific comorbid conditions, such as chronic kidney disease or heart failure, and recommend the use of ACEIs, ARBs, CCBs, or thiazide-type diuretics as initial therapy for most patients.
What lifestyle modifications are recommended by the JNC 8 guidelines for the management of hypertension?
+The guidelines recommend lifestyle modifications including dietary changes such as the DASH diet, increased physical activity, weight loss for those who are overweight or obese, and reduction in alcohol consumption.