The question of whether Nurse Practitioners (NPs) can prescribe medication is a multifaceted one, influenced by a variety of factors including jurisdiction, healthcare setting, and specific patient needs. In the United States, for example, the authority of NPs to prescribe medications varies from state to state, reflecting the complex interplay between state laws, professional regulations, and healthcare policies.
Legal Framework and Prescriptive Authority
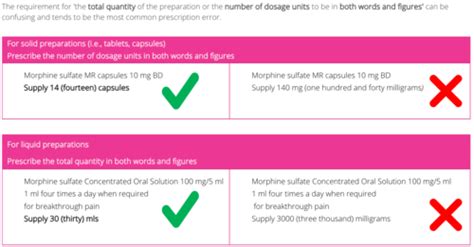
Generally, NPs are advanced practice registered nurses (APRNs) who have completed advanced education and training in the diagnosis and management of common medical conditions, including chronic illnesses. Their ability to prescribe medication is contingent upon their prescriptive authority, which is legally defined and can differ significantly across different jurisdictions. In some states, NPs have full prescriptive authority, allowing them to prescribe a wide range of medications, including controlled substances, without the need for physician supervision or collaboration. In contrast, other states may impose restrictions, requiring NPs to work under the supervision of a licensed physician or limiting the types of medications they can prescribe.
Prescriptive Authority by State
A detailed examination of state-specific laws and regulations reveals a spectrum of prescriptive authority for NPs. According to the American Association of Nurse Practitioners (AANP), as of 2022, all 50 states and the District of Columbia authorize NPs to prescribe medications, but the extent of this authority varies. For instance, some states allow NPs to prescribe controlled substances, while others do not. Understanding these variations is crucial for both NPs and patients, as it directly impacts the delivery of care and access to necessary medications.
| State | Prescriptive Authority |
|---|---|
| Full Practice States | NPs can prescribe without physician supervision or collaboration |
| Reduced Practice States | NPs can prescribe with physician supervision or collaboration |
| Restricted Practice States | NPs have limited prescriptive authority, often requiring physician supervision |

Professional and Patient Perspectives
Beyond the legal framework, the ability of NPs to prescribe medication also has significant implications for professional practice and patient care. From a professional standpoint, prescriptive authority is a critical component of NP practice, enabling them to provide comprehensive care that meets the full range of patient needs. For patients, the ability to receive prescriptions from NPs can enhance access to care, particularly in underserved or rural areas where physician availability may be limited. Moreover, the continuity of care provided by NPs, coupled with their prescriptive authority, can lead to better health outcomes and higher patient satisfaction.
Evidence-Based Practice and Outcomes
Research and clinical evidence support the notion that NPs, when granted prescriptive authority, can safely and effectively manage patient care, including prescribing medications. Studies have shown that outcomes for patients cared for by NPs are comparable to, if not better than, those for patients cared for by physicians, particularly in the context of primary care and chronic disease management. This evidence underscores the importance of NPs in the healthcare system and highlights the need for policies that support their full practice authority, including prescriptive authority.
Key Points
- NPs have the authority to prescribe medication in all 50 states and the District of Columbia, but the extent of this authority varies by state.
- Prescriptive authority for NPs is influenced by state laws, professional regulations, and healthcare policies.
- The ability of NPs to prescribe medication enhances access to care, particularly in underserved areas, and can lead to better health outcomes and patient satisfaction.
- Evidence supports the safe and effective management of patient care by NPs, including prescribing medications.
- Policies supporting full practice authority for NPs, including prescriptive authority, are critical for optimizing healthcare delivery and outcomes.
In conclusion, the ability of NPs to prescribe medication is a complex issue, influenced by legal, professional, and patient care considerations. As healthcare systems continue to evolve, with a growing emphasis on accessibility, quality, and cost-effectiveness, the role of NPs and their prescriptive authority will remain a vital component of healthcare policy and practice.
What is the current status of NP prescriptive authority in the United States?
+As of 2022, all 50 states and the District of Columbia authorize NPs to prescribe medications, but the extent of this authority varies by state, with some states granting full prescriptive authority and others imposing restrictions.
How does prescriptive authority impact patient care and outcomes?
+Prescriptive authority for NPs enhances access to care, particularly in underserved areas, and can lead to better health outcomes and patient satisfaction by allowing NPs to provide comprehensive care that meets the full range of patient needs.
What evidence supports the prescriptive authority of NPs?
+Research and clinical evidence demonstrate that NPs, when granted prescriptive authority, can safely and effectively manage patient care, including prescribing medications, with outcomes comparable to, if not better than, those for patients cared for by physicians.
This article has provided a comprehensive overview of the complex issue of NP prescriptive authority, highlighting its legal, professional, and patient care implications. By understanding the current status, evidence, and future directions of NP prescriptive authority, stakeholders can work towards optimizing healthcare delivery and outcomes.