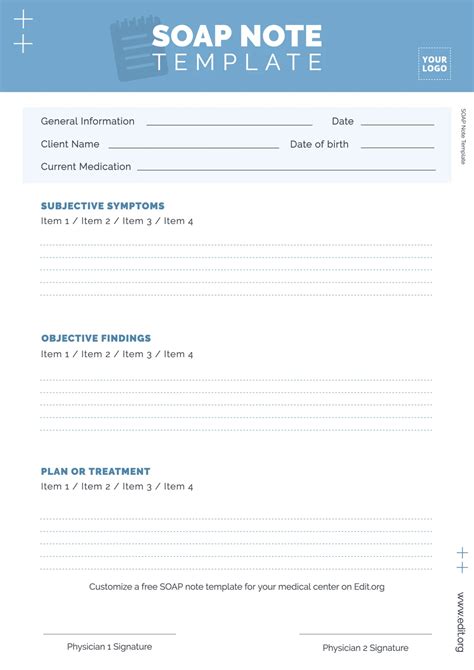
When it comes to maintaining accurate and detailed records of patient interactions, healthcare professionals rely on a standardized system known as SOAP notes. SOAP is an acronym that stands for Subjective, Objective, Assessment, and Plan, providing a structured format for documenting patient information. This template is crucial for ensuring that all relevant details are captured, facilitating effective communication among healthcare providers, and supporting high-quality patient care. In this article, we will delve into the components of a SOAP notes template, its significance in healthcare, and how it is used in practice.
Understanding the Components of SOAP Notes
The SOAP notes template is divided into four main sections, each serving a distinct purpose in the documentation process. Understanding these components is essential for effective use of the template.
Subjective Section
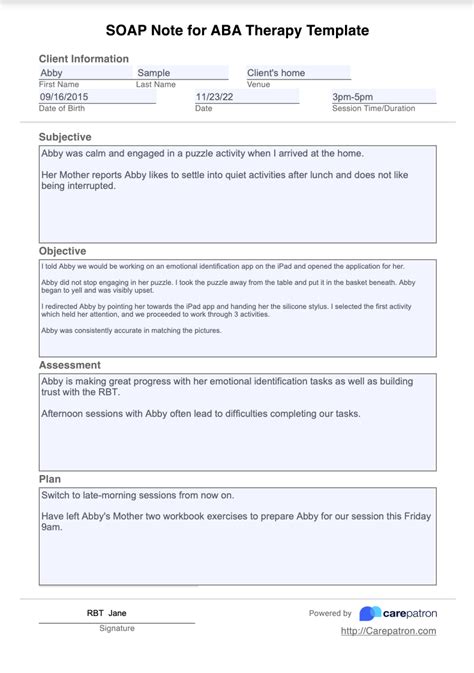
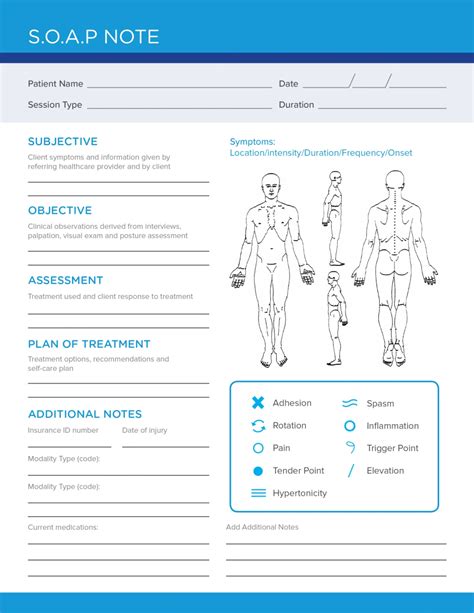
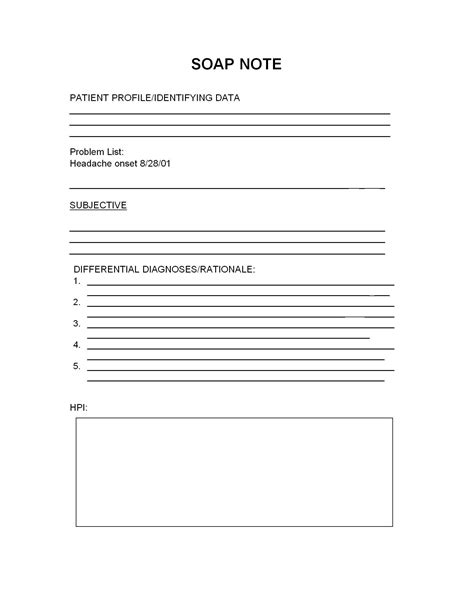
The subjective section of the SOAP notes template is where healthcare providers document the patient’s reported symptoms, concerns, and medical history. This information is gathered through patient interviews and is crucial for understanding the patient’s perspective on their condition. It includes details such as the chief complaint, history of present illness, past medical history, family history, and social history. The subjective information lays the groundwork for further investigation and diagnosis.
Objective Section
The objective section contains information that is observable and measurable by the healthcare provider. This includes vital signs, physical examination findings, laboratory results, and other diagnostic tests. The objective data provide concrete evidence of the patient’s condition, which, when combined with the subjective information, helps in forming a comprehensive picture of the patient’s health status.
Assessment Section
In the assessment section, healthcare providers interpret the subjective and objective data to arrive at a diagnosis or assessment of the patient’s condition. This section may include a list of potential diagnoses (differential diagnoses) and the healthcare provider’s impression of the patient’s condition based on the information gathered. The assessment is critical as it guides the development of the treatment plan.
Plan Section
The plan section outlines the actions to be taken to address the patient’s condition. This can include medication prescriptions, referrals to specialists, orders for further diagnostic tests, patient education, and follow-up appointments. The plan is tailored to the individual patient’s needs and is based on the assessment made in the previous section. It serves as a roadmap for the patient’s care and treatment.
| SOAP Component | Description |
|---|---|
| Subjective | Patient-reported symptoms and medical history |
| Objective | Observable and measurable data |
| Assessment | Diagnosis or condition assessment |
| Plan | Treatment plan and follow-up actions |
Key Points
- The SOAP notes template is a standardized method for documenting patient interactions.
- It consists of four sections: Subjective, Objective, Assessment, and Plan.
- Each section serves a distinct purpose in the patient care process.
- Effective use of SOAP notes enhances patient care quality and facilitates communication among healthcare providers.
- The template is adaptable to various healthcare settings and patient conditions.
The implementation of SOAP notes in healthcare practice has been shown to improve the quality of care by ensuring that all relevant information is systematically recorded and considered in the care process. By understanding and properly utilizing the SOAP notes template, healthcare providers can enhance patient outcomes, reduce errors, and contribute to a more efficient healthcare system.
Best Practices for Using SOAP Notes
While the SOAP notes template provides a structured approach to patient documentation, its effectiveness depends on how it is used. Best practices include ensuring that all sections are completed thoroughly and accurately, using clear and concise language, and reviewing and updating the notes regularly to reflect changes in the patient’s condition.
Importance of Clear Documentation
Clear and legible documentation is essential for effective communication among healthcare providers. It prevents misunderstandings and errors, ensuring that patient care is consistent and of high quality. Additionally, clear documentation supports legal and regulatory compliance, protecting both patients and healthcare providers.
Regular Review and Update
Patient conditions can change rapidly, making it crucial to review and update SOAP notes regularly. This ensures that the documentation remains relevant and accurate, reflecting the current state of the patient’s health and the evolving treatment plan.
What is the primary purpose of SOAP notes in healthcare?
+The primary purpose of SOAP notes is to provide a standardized method for documenting patient information, facilitating effective communication among healthcare providers, and supporting high-quality patient care.
How do SOAP notes contribute to patient care quality?
+SOAP notes contribute to patient care quality by ensuring that all relevant patient information is systematically recorded and considered, reducing errors, and enhancing communication among healthcare providers.
What are the key components of a SOAP notes template?
+The key components of a SOAP notes template are the Subjective, Objective, Assessment, and Plan sections, each serving a distinct purpose in the patient care process.
In conclusion, the SOAP notes template is a vital tool in healthcare, providing a structured approach to patient documentation that enhances care quality, facilitates communication, and supports regulatory compliance. By understanding the components of SOAP notes and implementing best practices in their use, healthcare providers can deliver more effective and personalized care, ultimately improving patient outcomes.