When it comes to documenting patient interactions, accuracy and clarity are paramount. One of the most commonly used methods for recording patient information is the SOAP note. Developed by Dr. Lawrence Weed in the 1960s, SOAP stands for Subjective, Objective, Assessment, and Plan, providing a structured format for healthcare professionals to detail patient data. Effective use of SOAP notes not only enhances patient care but also aids in legal protection and facilitates communication among healthcare providers. Here are five tips for creating comprehensive and useful SOAP notes:
Key Points
- Ensure accuracy and completeness in the subjective section by including all relevant patient statements.
- Be thorough and objective in documenting observations and measurements.
- Utilize the assessment section to analyze the data collected and formulate a diagnosis or problem list.
- Develop a clear, patient-centered plan that includes specific interventions and follow-up actions.
- Regularly review and update SOAP notes to reflect changes in patient condition and treatment outcomes.
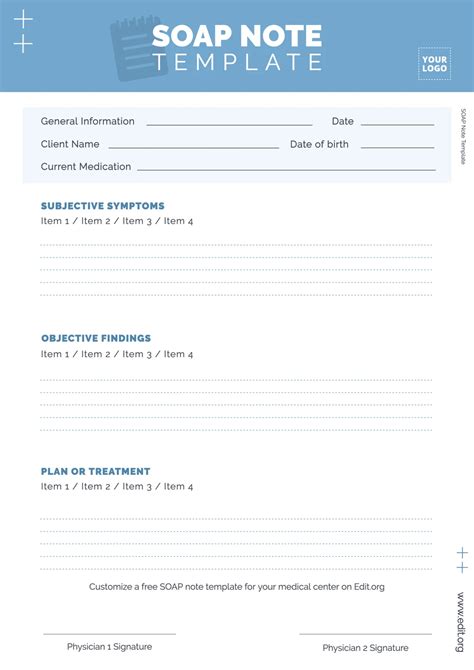
Understanding the Components of a SOAP Note
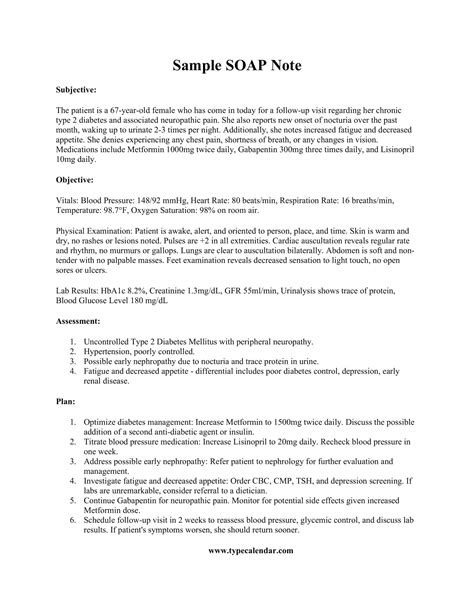
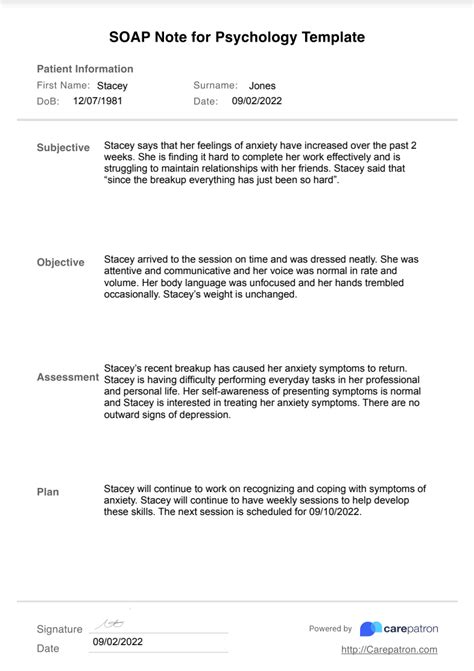
The subjective section of a SOAP note involves documenting the patient’s reported symptoms, medical history, and any other relevant information they provide. It’s crucial to record these details accurately, using quotes when possible to capture the patient’s exact words. This not only helps in understanding the patient’s condition but also in establishing a rapport and ensuring that their concerns are addressed. For instance, if a patient reports experiencing “sharp pains in the chest,” this should be noted verbatim to avoid any potential misinterpretation.
Objective Findings and Their Importance
The objective section is where healthcare providers document their observations, measurements, and the results of any diagnostic tests. This can include vital signs, lab results, and physical examination findings. Being thorough and precise in this section is vital, as it provides quantifiable data that can be used to assess the patient’s condition and monitor progress over time. For example, instead of simply stating that a patient has a fever, the SOAP note should specify the temperature, e.g., “The patient’s temperature is 38.5°C.” This level of detail is essential for making informed decisions about care.
| SOAP Component | Description |
|---|---|
| Subjective | Patient-reported symptoms and medical history |
| Objective | Healthcare provider's observations and diagnostic test results |
| Assessment | Analysis of the data to formulate a diagnosis or problem list |
| Plan | Specific interventions and follow-up actions for the patient |
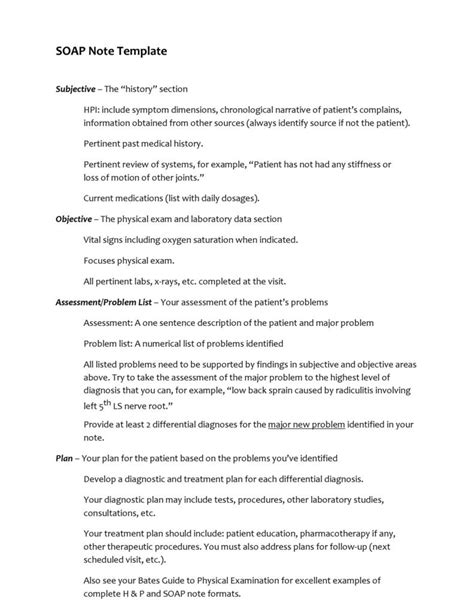
Best Practices for SOAP Note Documentation
Writing effective SOAP notes requires a combination of technical knowledge, attention to detail, and the ability to communicate complex information clearly. Healthcare professionals should strive to be as specific as possible, avoiding vague terms and focusing on quantifiable data. Regular review of SOAP notes can also help in identifying patterns or areas where patient care might be improved. Furthermore, staying updated with the latest clinical guidelines and best practices is crucial for ensuring that the care provided is evidence-based and aligned with current standards.
Enhancing Patient Care Through Clear Communication
Clear and comprehensive SOAP notes are not just about documentation; they are a tool for enhancing patient care. By providing a detailed, structured account of a patient’s condition and treatment plan, healthcare providers can ensure continuity of care, even when the patient is seen by different members of the healthcare team. This clarity also helps in minimizing errors and ensuring that all interventions are patient-centered and evidence-based. For example, a SOAP note that clearly outlines a patient’s medication regimen and any potential side effects can help prevent drug interactions and ensure that the patient receives the correct treatment.
In conclusion, SOAP notes are a fundamental tool in healthcare, offering a structured approach to patient documentation that enhances care quality, facilitates communication, and supports legal and professional standards. By following the tips outlined and adopting best practices in SOAP note writing, healthcare professionals can ensure that their documentation is not only compliant but also contributes positively to patient outcomes.
What is the primary purpose of a SOAP note?
+The primary purpose of a SOAP note is to provide a structured format for documenting patient information, including subjective and objective data, assessment, and plan, to enhance patient care and communication among healthcare providers.
How often should SOAP notes be updated?
+SOAP notes should be updated regularly to reflect changes in the patient’s condition, new diagnostic findings, and any adjustments to the treatment plan. The frequency of updates can vary depending on the patient’s needs and the healthcare setting.
What are the key components of a SOAP note?
+The key components of a SOAP note include the subjective section (patient-reported information), the objective section (healthcare provider’s observations and test results), the assessment section (analysis and diagnosis), and the plan section (treatment and follow-up actions).