When it comes to maintaining accurate and comprehensive patient records, the SOAP note has become an indispensable tool in the healthcare industry. Developed by Dr. Lawrence Weed in the 1960s, the SOAP note is a standardized method of documenting patient information in a clear and organized manner. The acronym SOAP stands for Subjective, Objective, Assessment, and Plan, which are the four primary components of this note-taking system. In this article, we will delve into the world of SOAP notes, exploring their significance, the benefits they offer, and most importantly, providing 5 valuable tips on how to write effective SOAP notes.
Key Points
- Understanding the SOAP note format and its components
- Importance of clear and concise language in SOAP notes
- Accurate documentation of patient subjective and objective information
- Developing a comprehensive assessment and plan
- Regular review and update of SOAP notes for continuous patient care
Understanding the SOAP Note Format
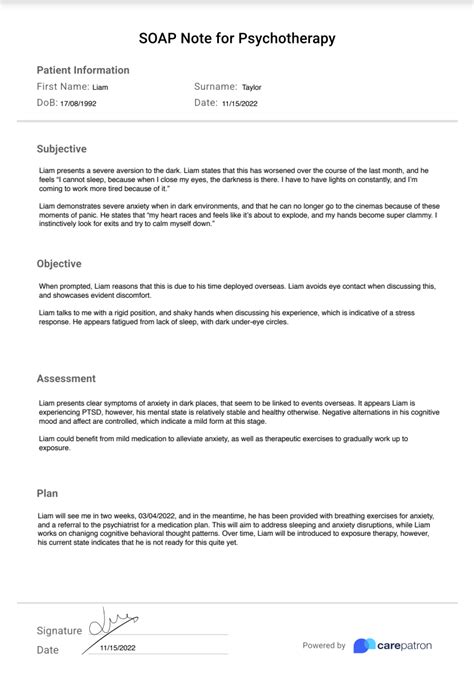
The SOAP note format is designed to ensure that all relevant information about a patient’s visit is captured in a structured and easily accessible way. The subjective component involves documenting the patient’s reported symptoms, medical history, and any concerns they may have. This is followed by the objective section, where healthcare providers record observable and measurable data, such as vital signs, laboratory results, and physical examination findings. The assessment section is where the healthcare provider interprets the information gathered, making a diagnosis or identifying potential issues. Lastly, the plan outlines the actions to be taken, including treatments, medications, lifestyle changes, and follow-up appointments.
Tip 1: Use Clear and Concise Language
One of the most critical aspects of writing effective SOAP notes is using language that is both clear and concise. Healthcare providers should avoid using jargon or complex medical terminology that might confuse other caregivers or the patient themselves. Instead, focusing on simple, straightforward language ensures that the information conveyed is easily understandable, reducing the risk of misinterpretation and enhancing patient care.
Tip 2: Document Subjective Information Accurately
The subjective component of the SOAP note is crucial as it provides insight into the patient’s perspective on their condition. Healthcare providers should strive to document this information accurately, quoting the patient’s words whenever possible to maintain the integrity of their concerns and symptoms. This not only helps in building trust with the patient but also ensures that their needs are addressed comprehensively.
Tip 3: Focus on Objective Data
The objective section of the SOAP note is where measurable and observable data are recorded. This includes vital signs, laboratory results, and findings from physical examinations. It is essential to be meticulous in documenting this information, as it forms the basis of the assessment and subsequent plan. Healthcare providers should ensure that all data are accurately recorded and dated, providing a clear timeline of the patient’s progress.
Tip 4: Develop a Comprehensive Assessment and Plan
The assessment and plan sections of the SOAP note are where the healthcare provider synthesizes the information gathered to make a diagnosis or identify issues and then outlines the steps to be taken. Developing a comprehensive assessment involves considering all the subjective and objective information, as well as any previous medical history or treatments. The plan should be tailored to the individual patient’s needs, including specific interventions, medications, and follow-up care. It is also crucial to involve the patient in this process, educating them about their condition and the proposed treatment plan to ensure compliance and optimal outcomes.
| SOAP Component | Key Considerations |
|---|---|
| Subjective | Accurate quotation of patient's words, comprehensive documentation of symptoms and concerns |
| Objective | Precise recording of measurable data, inclusion of all relevant test results |
| Assessment | Integration of subjective and objective data, consideration of patient's medical history |
| Plan | Personalized treatment approach, clear instructions for patient, schedule for follow-up |

Tip 5: Regular Review and Update of SOAP Notes
Finally, it is vital to regularly review and update SOAP notes to reflect the ongoing care of the patient. This ensures that all healthcare providers involved in the patient’s care have access to the most current and comprehensive information, facilitating coordinated and effective care. Regular updates also help in tracking the patient’s progress over time, allowing for adjustments to the treatment plan as necessary.
What is the primary purpose of a SOAP note?
+The primary purpose of a SOAP note is to provide a standardized method of documenting patient information in a clear and organized manner, facilitating effective communication among healthcare providers and enhancing patient care.
How often should SOAP notes be updated?
+SOAP notes should be updated regularly, ideally after each patient visit or encounter, to ensure that they reflect the current status of the patient's condition and care plan.
What are the benefits of using SOAP notes in patient care?
+The benefits of using SOAP notes include improved communication among healthcare providers, enhanced patient care through comprehensive and accurate documentation, and better outcomes due to tailored treatment plans.
In conclusion, writing effective SOAP notes is a critical skill for healthcare providers, ensuring that patient care is well-documented, coordinated, and of the highest quality. By following the 5 tips outlined above, healthcare professionals can enhance their SOAP note writing skills, ultimately contributing to better patient outcomes and more efficient healthcare delivery.