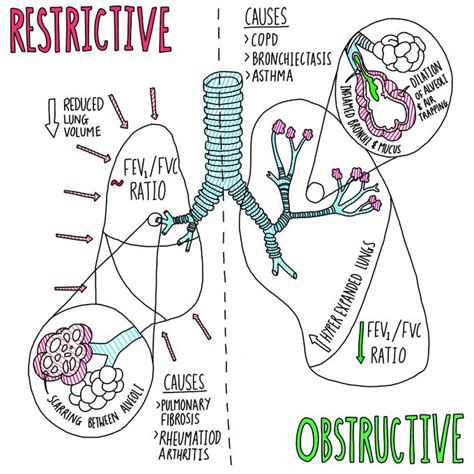
Obstructive and restrictive airway diseases are two distinct categories of respiratory disorders that affect the lungs and airways, leading to breathing difficulties. Understanding the differences between these two types of diseases is crucial for accurate diagnosis, effective treatment, and improved patient outcomes. In this article, we will delve into the characteristics, causes, symptoms, and management strategies of obstructive and restrictive airway diseases, highlighting their distinct features and implications for patient care.
Key Points
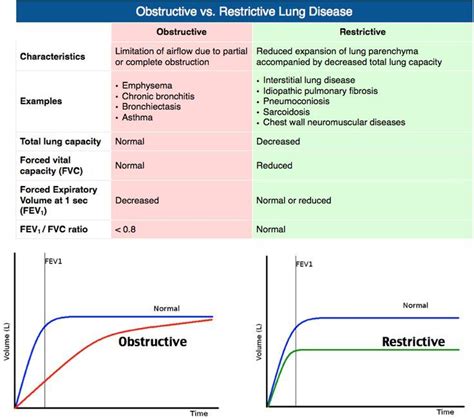
- Obstructive airway diseases, such as chronic obstructive pulmonary disease (COPD) and asthma, are characterized by airway inflammation and obstruction, leading to breathing difficulties.
- Restrictive airway diseases, including idiopathic pulmonary fibrosis (IPF) and sarcoidosis, are marked by inflammation and scarring of lung tissue, resulting in reduced lung volume and capacity.
- Accurate diagnosis of obstructive and restrictive airway diseases requires a comprehensive evaluation, including medical history, physical examination, pulmonary function tests, and imaging studies.
- Treatment strategies for obstructive and restrictive airway diseases differ, with obstructive diseases often managed with bronchodilators and corticosteroids, and restrictive diseases treated with anti-fibrotic agents and oxygen therapy.
- Early recognition and management of obstructive and restrictive airway diseases can significantly improve patient outcomes, reducing morbidity and mortality associated with these conditions.
Obstructive Airway Diseases
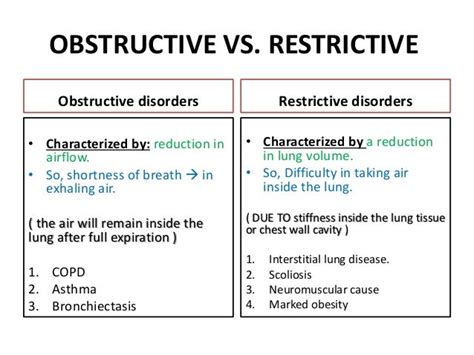
Obstructive airway diseases are characterized by inflammation and obstruction of the airways, leading to breathing difficulties. The most common obstructive airway diseases are chronic obstructive pulmonary disease (COPD) and asthma. COPD is a progressive disease caused by long-term exposure to lung irritants, such as cigarette smoke, air pollution, and occupational hazards. Asthma, on the other hand, is a chronic inflammatory disease of the airways, often triggered by allergens, respiratory infections, or environmental factors.
The pathophysiology of obstructive airway diseases involves airway inflammation, bronchospasm, and mucus production, resulting in narrowed airways and impaired gas exchange. Symptoms of obstructive airway diseases include wheezing, coughing, shortness of breath, and chest tightness. Pulmonary function tests, such as spirometry and plethysmography, are essential for diagnosing obstructive airway diseases, as they measure lung function and airway obstruction.
Causes and Risk Factors
The causes and risk factors for obstructive airway diseases are multifactorial. Smoking is the leading cause of COPD, while asthma is often triggered by allergens, respiratory infections, or environmental factors. Other risk factors for obstructive airway diseases include air pollution, occupational exposures, and genetic predisposition. Understanding these causes and risk factors is crucial for developing effective prevention and treatment strategies.
| Obstructive Airway Disease | Cause | Risk Factor |
|---|---|---|
| COPD | Long-term exposure to lung irritants | Smoking, air pollution, occupational hazards |
| Asthma | Chronic inflammatory disease of the airways | Allergens, respiratory infections, environmental factors |
Restrictive Airway Diseases
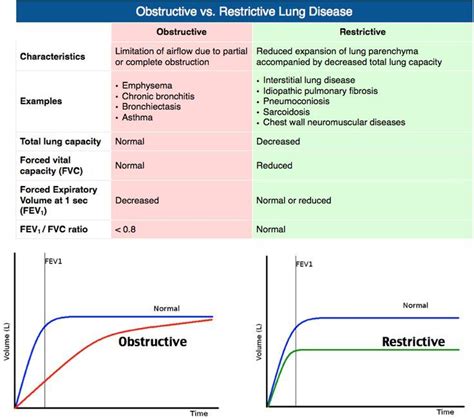
Restrictive airway diseases, also known as interstitial lung diseases, are characterized by inflammation and scarring of lung tissue, resulting in reduced lung volume and capacity. The most common restrictive airway diseases are idiopathic pulmonary fibrosis (IPF) and sarcoidosis. IPF is a chronic and progressive disease of unknown cause, while sarcoidosis is a systemic inflammatory disease that affects multiple organs, including the lungs.
The pathophysiology of restrictive airway diseases involves inflammation and fibrosis of lung tissue, leading to reduced lung elasticity and impaired gas exchange. Symptoms of restrictive airway diseases include shortness of breath, coughing, and chest pain. Imaging studies, such as high-resolution computed tomography (HRCT) and pulmonary function tests, are essential for diagnosing restrictive airway diseases, as they evaluate lung structure and function.
Diagnosis and Management
Diagnosing obstructive and restrictive airway diseases requires a comprehensive evaluation, including medical history, physical examination, pulmonary function tests, and imaging studies. Treatment strategies for obstructive and restrictive airway diseases differ, with obstructive diseases often managed with bronchodilators and corticosteroids, and restrictive diseases treated with anti-fibrotic agents and oxygen therapy. Early recognition and management of these diseases can significantly improve patient outcomes, reducing morbidity and mortality associated with these conditions.
Comparison of Obstructive and Restrictive Airway Diseases
A comparison of obstructive and restrictive airway diseases highlights their distinct features and implications for patient care. Obstructive airway diseases are characterized by airway inflammation and obstruction, while restrictive airway diseases are marked by inflammation and scarring of lung tissue. Understanding these differences is crucial for developing effective diagnosis and treatment strategies, as well as improving patient outcomes.
| Disease | Characteristics | Symptoms | Treatment |
|---|---|---|---|
| Obstructive Airway Disease | Airway inflammation and obstruction | Wheezing, coughing, shortness of breath | Bronchodilators, corticosteroids |
| Restrictive Airway Disease | Inflammation and scarring of lung tissue | Shortness of breath, coughing, chest pain | Anti-fibrotic agents, oxygen therapy |
What is the main difference between obstructive and restrictive airway diseases?
+The main difference between obstructive and restrictive airway diseases is the location and nature of the disease process. Obstructive airway diseases involve airway inflammation and obstruction, while restrictive airway diseases involve inflammation and scarring of lung tissue.
How are obstructive and restrictive airway diseases diagnosed?
+Diagnosing obstructive and restrictive airway diseases requires a comprehensive evaluation, including medical history, physical examination, pulmonary function tests, and imaging studies. Pulmonary function tests, such as spirometry and plethysmography, are essential for diagnosing obstructive airway diseases, while imaging studies, such as HRCT, are crucial for diagnosing restrictive airway diseases.
What are the treatment options for obstructive and restrictive airway diseases?
+Treatment strategies for obstructive and restrictive airway diseases differ. Obstructive airway diseases are often managed with bronchodilators and corticosteroids, while restrictive airway diseases are treated with anti-fibrotic agents and oxygen therapy. Early recognition and management of these diseases can significantly improve patient outcomes, reducing morbidity and mortality associated with these conditions.
In conclusion, obstructive and restrictive airway diseases are two distinct categories of respiratory disorders that require accurate diagnosis and effective treatment. By understanding the characteristics, causes, symptoms, and management strategies of these diseases, healthcare providers can develop tailored approaches to meet the unique needs of each patient, ultimately enhancing the quality of care and reducing the burden of these diseases. Meta description: Learn about the differences between obstructive and restrictive airway diseases, including their characteristics, causes, symptoms, and treatment options.