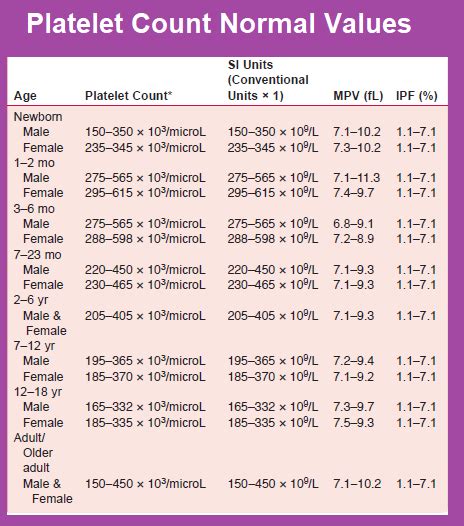
The normal platelet count in humans varies by age, with significant changes occurring during the first few years of life and more subtle adjustments throughout adulthood. Understanding these age-related fluctuations is crucial for accurate diagnosis and treatment of various hematological conditions. Platelets, also known as thrombocytes, play a vital role in blood clotting and are produced in the bone marrow. Their count can be influenced by a range of factors including age, lifestyle, and underlying health conditions.
Platelet Count Ranges by Age Group
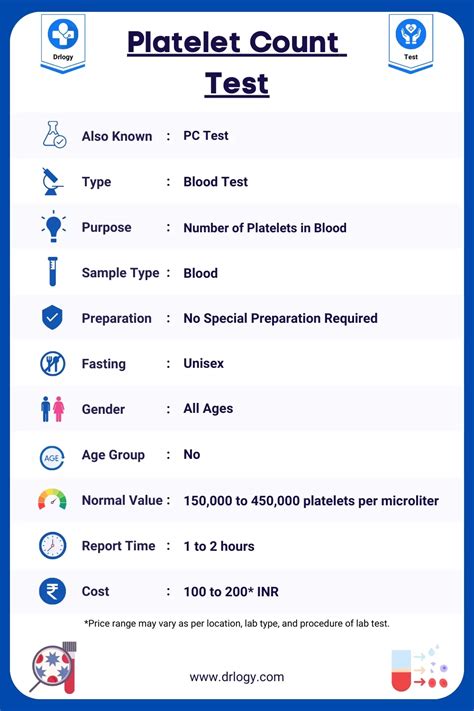
A comprehensive analysis of platelet counts across different age groups reveals distinct patterns. Infants and young children tend to have higher platelet counts compared to adults. According to the American Academy of Pediatrics and other medical guidelines, the normal platelet count ranges are as follows:
| Age Group | Normal Platelet Count Range (x10^9/L) |
|---|---|
| Newborns (0-1 week) | 100-300 |
| Infants (1-12 months) | 150-450 |
| Children (1-5 years) | 150-450 |
| Children (6-12 years) | 150-400 |
| Adolescents (13-18 years) | 150-400 |
| Adults | 150-450 |
| Elderly (65+ years) | 100-400 |
Understanding Platelet Count Variations
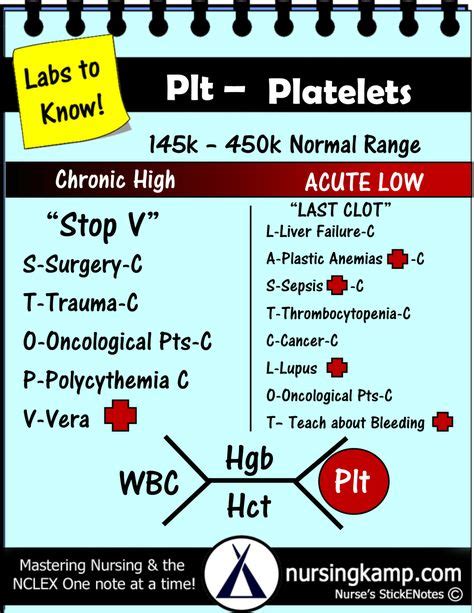
Platelet counts can vary significantly among individuals of the same age group due to various genetic and environmental factors. Lifestyle choices, such as smoking and alcohol consumption, can affect platelet production and function. Additionally, certain medications, like aspirin, can influence platelet activity. It is essential to consider these factors when interpreting platelet count results. For instance, a study published in the Journal of Clinical Oncology found that smokers tend to have higher platelet counts than non-smokers, which could be a factor in the increased risk of thrombotic events observed in smokers.
Key Points
- Platelet count varies by age, with infants and young children having higher counts than adults.
- Lifestyle factors such as smoking and alcohol consumption can affect platelet count and function.
- Certain medications can influence platelet activity, necessitating careful consideration in clinical practice.
- Genetic predispositions can also play a role in determining an individual's platelet count.
- Reference ranges for platelet counts can vary slightly between different laboratories, emphasizing the need for standardized testing protocols.
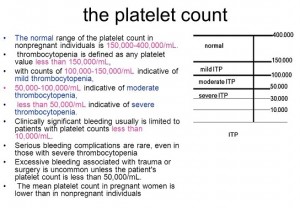
Clinical Significance of Platelet Counts
The clinical significance of platelet counts lies in their role in diagnosing and managing various conditions. Thrombocytopenia, characterized by a low platelet count, can increase the risk of bleeding, while thrombocytosis, or a high platelet count, can predispose to thrombotic events. A balanced platelet count is crucial for maintaining normal hemostasis. For example, a patient with a low platelet count may require adjustments in their medication regimen or may need to undergo platelet transfusions to prevent or manage bleeding complications.
Age-Related Considerations in Platelet-Related Disorders
Age is a critical factor in the diagnosis and treatment of platelet-related disorders. In newborns, thrombocytopenia can be due to maternal factors, such as immune thrombocytopenia purpura (ITP), or congenital infections. In adults, lifestyle factors and underlying health conditions, such as liver disease or myeloproliferative neoplasms, can influence platelet counts. Age-specific considerations are essential for developing effective treatment plans. For instance, elderly patients with thrombocytosis may require more aggressive management due to their increased risk of cardiovascular events.
Diagnostic Approaches and Treatment Strategies
The diagnosis of platelet count abnormalities typically involves a complete blood count (CBC) with platelet count, followed by additional tests to determine the underlying cause. Treatment strategies vary depending on the cause and severity of the condition. For thrombocytopenia, treatments may include platelet transfusions, medications to stimulate platelet production, or addressing underlying conditions. For thrombocytosis, treatment often focuses on reducing the risk of thrombotic events through antiplatelet therapy or medications that decrease platelet production.
Future Directions in Platelet Count Management
Advances in medical technology and a deeper understanding of platelet biology are expected to improve the management of platelet count abnormalities. Personalized medicine approaches, taking into account an individual’s genetic profile, lifestyle, and comorbid conditions, may offer more targeted and effective treatments. Additionally, research into novel therapeutic agents and the development of more sensitive diagnostic tools will further refine the clinical management of platelet-related disorders.
What is the normal range for platelet count in adults?
+The normal range for platelet count in adults is generally considered to be between 150 and 450 x10^9/L, though this can vary slightly depending on the laboratory.
Can lifestyle factors affect platelet count?
+Yes, lifestyle factors such as smoking, alcohol consumption, and physical activity can influence platelet count and function.
What are the implications of an abnormal platelet count?
+An abnormal platelet count can increase the risk of bleeding or thrombotic events, depending on whether the count is low (thrombocytopenia) or high (thrombocytosis), respectively.
In conclusion, understanding the normal platelet count ranges by age and the factors that influence these counts is essential for the accurate diagnosis and management of platelet-related disorders. As medical knowledge and technologies continue to evolve, so too will our ability to personalize care and improve outcomes for individuals with abnormalities in their platelet counts.