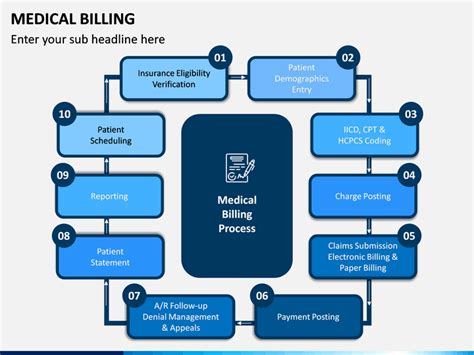
The medical billing process is a complex and crucial aspect of healthcare administration, requiring precision, attention to detail, and a thorough understanding of regulatory requirements. As the healthcare landscape continues to evolve, medical billing professionals must stay up-to-date with the latest developments and best practices to ensure efficient and effective revenue cycle management. In this article, we will explore five essential medical billing tips, providing valuable insights and expert advice for healthcare professionals seeking to optimize their billing operations.
Key Points
- Accurate patient registration and data collection are critical for successful medical billing
- Understanding and adhering to coding guidelines and regulations is essential for compliant billing practices
- Effective claims submission and follow-up procedures can significantly reduce denial rates and improve revenue cycle efficiency
- Regular auditing and monitoring of billing processes can help identify areas for improvement and minimize errors
- Staying current with industry developments and updates is vital for maintaining compliant and efficient medical billing operations
Tip 1: Ensure Accurate Patient Registration and Data Collection

The foundation of successful medical billing lies in accurate patient registration and data collection. This includes verifying patient demographics, insurance information, and medical history. Accurate data entry is crucial, as errors can lead to denied claims, delayed payments, and even legal issues. Healthcare providers should implement robust data collection processes, including electronic health records (EHRs) and patient registration systems, to ensure the accuracy and completeness of patient information. According to a study by the American Academy of Professional Coders (AAPC), accurate patient registration can reduce claim denials by up to 30%.
Importance of Verification
Verification of patient information is a critical step in the medical billing process. This includes verifying insurance coverage, deductibles, and copayments, as well as ensuring that patient demographics and contact information are up-to-date. Eligibility verification can help prevent claim denials and reduce the risk of non-payment. Healthcare providers should invest in automated verification tools and train staff to perform thorough verification checks to ensure the accuracy of patient information.
| Verification Type | Frequency |
|---|---|
| Insurance Verification | Before each visit |
| Demographic Verification | At least quarterly |
| Eligibility Verification | Before each claim submission |
Tip 2: Understand and Adhere to Coding Guidelines and Regulations

Medical coding is a critical aspect of medical billing, and understanding coding guidelines and regulations is essential for compliant billing practices. Healthcare providers must stay up-to-date with the latest coding updates, including ICD-10 and CPT codes, to ensure accurate and compliant coding. The Centers for Medicare and Medicaid Services (CMS) provides regular updates and guidance on coding regulations, and healthcare providers should invest in ongoing education and training to ensure that staff are knowledgeable and proficient in coding guidelines.
Coding Compliance
Coding compliance is critical to prevent claim denials and audits. Healthcare providers should implement robust coding compliance programs, including regular audits and monitoring, to ensure that coding practices are accurate and compliant. Coding audits can help identify areas for improvement and minimize errors, reducing the risk of non-payment and reputational damage. According to a study by the Healthcare Financial Management Association (HFMA), coding compliance programs can reduce claim denials by up to 25%.
Tip 3: Implement Effective Claims Submission and Follow-up Procedures
Effective claims submission and follow-up procedures are critical to reducing denial rates and improving revenue cycle efficiency. Healthcare providers should invest in automated claims submission systems and train staff to perform thorough follow-up checks to ensure that claims are processed efficiently and accurately. Claims tracking can help identify issues and minimize delays, reducing the risk of non-payment and improving cash flow.
Follow-up Procedures
Follow-up procedures are essential to ensuring that claims are processed efficiently and accurately. This includes tracking claims status, responding to payer inquiries, and resolving issues promptly. Claims follow-up can help reduce denial rates, minimize delays, and improve revenue cycle efficiency. Healthcare providers should invest in automated follow-up systems and train staff to perform thorough follow-up checks to ensure that claims are processed efficiently and accurately.
Tip 4: Regularly Audit and Monitor Billing Processes
Regular auditing and monitoring of billing processes are critical to identifying areas for improvement and minimizing errors. Healthcare providers should implement robust auditing and monitoring programs, including regular reviews of claims data, to ensure that billing practices are accurate and compliant. Auditing and monitoring can help identify issues, reduce denial rates, and improve revenue cycle efficiency. According to a study by the American Medical Association (AMA), regular auditing and monitoring can reduce claim denials by up to 20%.
Auditing and Monitoring
Auditing and monitoring are essential to ensuring that billing practices are accurate and compliant. This includes regular reviews of claims data, coding practices, and patient registration information. Auditing and monitoring programs can help identify areas for improvement, reduce denial rates, and improve revenue cycle efficiency. Healthcare providers should invest in automated auditing and monitoring systems and train staff to perform thorough reviews to ensure that billing practices are accurate and compliant.
Tip 5: Stay Current with Industry Developments and Updates

Staying current with industry developments and updates is vital for maintaining compliant and efficient medical billing operations. Healthcare providers should invest in ongoing education and training, including regular updates on coding guidelines, regulatory requirements, and industry best practices. Industry updates can help healthcare providers stay ahead of the curve, reduce errors, and improve revenue cycle efficiency. According to a study by the Medical Group Management Association (MGMA), ongoing education and training can reduce claim denials by up to 15%.
What are the most common causes of medical billing errors?
+The most common causes of medical billing errors include inaccurate patient registration, incorrect coding, and insufficient documentation. To minimize errors, healthcare providers should implement robust data collection processes, invest in ongoing education and training, and perform regular audits and monitoring.
How can healthcare providers improve their medical billing operations?
+Healthcare providers can improve their medical billing operations by implementing accurate patient registration and data collection processes, understanding and adhering to coding guidelines and regulations, and investing in ongoing education and training. Regular auditing and monitoring, as well as effective claims submission and follow-up procedures, can also help reduce denial rates and improve revenue cycle efficiency.
What are the benefits of automated medical billing systems?
+Automated medical billing systems can help reduce errors, improve revenue cycle efficiency, and minimize delays. These systems can also help healthcare providers stay current with industry developments and updates, reduce claim denials, and improve patient satisfaction. By investing in automated medical billing systems, healthcare providers can streamline their billing operations, reduce costs, and improve overall efficiency.
In conclusion, medical billing is a complex and critical aspect of healthcare administration, requiring precision, attention to detail, and a thorough understanding of regulatory requirements. By following these five essential medical billing tips, healthcare providers can optimize their billing operations, reduce errors, and improve revenue cycle efficiency. Remember to stay current with industry developments and updates, invest in ongoing education and training, and implement robust auditing and monitoring programs to ensure compliant and efficient medical billing operations.