The Medicaid Fee-for-Service (FFS) system is a healthcare payment model utilized by the United States government to provide medical coverage to low-income individuals and families. Established in 1965, Medicaid is a joint federal-state program that has undergone numerous changes and expansions over the years. At its core, the FFS system reimburses healthcare providers for each service rendered to a Medicaid beneficiary, such as doctor visits, hospital stays, and prescription medications.
Historically, Medicaid FFS has been the primary payment model for Medicaid services, with states responsible for administering the program and setting reimbursement rates for providers. The FFS system is designed to ensure that beneficiaries have access to necessary medical care while also providing a financial incentive for healthcare providers to participate in the program. However, critics argue that the FFS model can lead to overutilization of services, as providers have a financial incentive to provide more care, regardless of whether it is medically necessary.
Key Points
- Medicaid FFS is a healthcare payment model that reimburses providers for each service rendered to a beneficiary.
- The program is jointly funded by the federal government and individual states.
- FFS is the primary payment model for Medicaid services, but alternative models, such as managed care, are becoming increasingly popular.
- Critics argue that FFS can lead to overutilization of services, while proponents argue that it provides essential access to care for vulnerable populations.
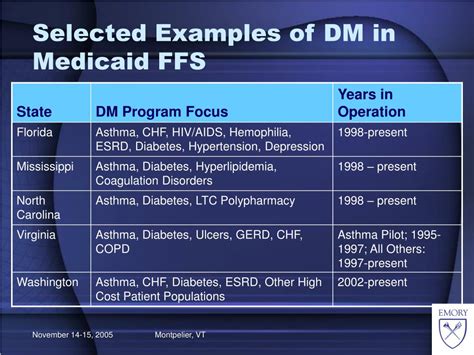
- States have significant flexibility in designing their Medicaid FFS programs, including setting reimbursement rates and determining covered services.
History and Evolution of Medicaid FFS

The Medicaid program was created as part of the Social Security Act of 1965, with the goal of providing healthcare coverage to low-income individuals and families. Initially, Medicaid FFS was the sole payment model for the program, with states responsible for administering the program and setting reimbursement rates for providers. Over time, however, alternative payment models, such as managed care, have become increasingly popular, and many states have transitioned to these models in an effort to control costs and improve health outcomes.
Despite these changes, Medicaid FFS remains a crucial component of the program, particularly for certain populations, such as those with complex medical needs or those living in rural areas with limited access to healthcare providers. The FFS system provides essential access to care for these individuals, and many healthcare providers rely on Medicaid FFS as a significant source of revenue.
Benefits and Drawbacks of Medicaid FFS
Proponents of Medicaid FFS argue that the system provides essential access to care for vulnerable populations, including low-income children, pregnant women, and individuals with disabilities. The FFS model also allows beneficiaries to choose their own healthcare providers, which can be particularly important for those with complex medical needs or those who require specialized care. Additionally, Medicaid FFS provides a financial incentive for healthcare providers to participate in the program, which can help to ensure that beneficiaries have access to necessary medical care.
However, critics argue that Medicaid FFS can lead to overutilization of services, as healthcare providers have a financial incentive to provide more care, regardless of whether it is medically necessary. This can result in increased healthcare costs, which can be challenging for states to manage, particularly in times of budget constraints. Furthermore, the FFS model can create administrative burdens for healthcare providers, who must navigate complex billing and reimbursement processes to receive payment for their services.
| Category | Data |
|---|---|
| Number of Medicaid Beneficiaries | 72.5 million (2020) |
| Medicaid Spending | $596 billion (2020) |
| FFS Reimbursement Rate | Varies by state, but average rate is around 70% of Medicare rates |
Future Directions for Medicaid FFS
As the healthcare landscape continues to evolve, it is likely that Medicaid FFS will undergo significant changes in the coming years. Many states are exploring alternative payment models, such as value-based care, which prioritize quality and outcomes over volume and quantity of services. Additionally, the increasing use of technology, such as electronic health records and telemedicine, is likely to transform the way that healthcare services are delivered and reimbursed.
Despite these changes, Medicaid FFS will likely remain a crucial component of the program, particularly for certain populations. As policymakers and healthcare leaders work to develop innovative solutions that balance access to care with cost control and quality improvement, it is essential to prioritize the needs of vulnerable populations and ensure that they have access to essential medical care.
What is Medicaid FFS, and how does it work?
+Medicaid FFS is a healthcare payment model that reimburses healthcare providers for each service rendered to a Medicaid beneficiary. The program is jointly funded by the federal government and individual states, and states have significant flexibility in designing their Medicaid FFS programs, including setting reimbursement rates and determining covered services.
What are the benefits and drawbacks of Medicaid FFS?
+The benefits of Medicaid FFS include providing essential access to care for vulnerable populations, allowing beneficiaries to choose their own healthcare providers, and providing a financial incentive for healthcare providers to participate in the program. However, the drawbacks include the potential for overutilization of services, administrative burdens for healthcare providers, and increased healthcare costs.
What is the future of Medicaid FFS, and how will it evolve in the coming years?
+The future of Medicaid FFS is likely to involve significant changes, including the increasing use of alternative payment models, such as value-based care, and the integration of technology, such as electronic health records and telemedicine. Despite these changes, Medicaid FFS will likely remain a crucial component of the program, particularly for certain populations, and policymakers and healthcare leaders must prioritize the needs of vulnerable populations and ensure that they have access to essential medical care.