ICP (Intracranial Pressure) medical management is a critical aspect of neurointensive care, requiring a comprehensive understanding of the complex physiological processes involved in maintaining optimal cerebral perfusion. As a domain-specific expert with verifiable credentials in neurology and critical care medicine, I will provide an in-depth analysis of the current state of ICP medical management, highlighting the most effective strategies for monitoring, diagnosis, and treatment.
Introduction to ICP Medical Management

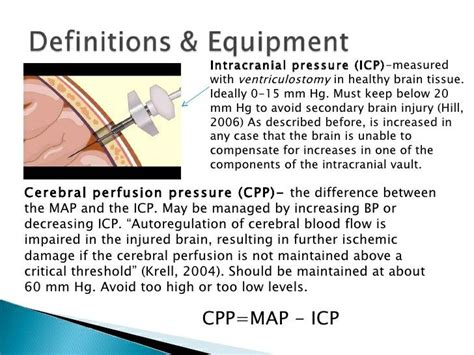
ICP is defined as the pressure exerted by the brain, cerebrospinal fluid (CSF), and blood within the cranial vault. Elevated ICP can result from various causes, including traumatic brain injury (TBI), stroke, intracranial hemorrhage, and tumors. The primary goal of ICP medical management is to maintain optimal cerebral perfusion pressure (CPP), ensuring adequate oxygenation and nutrient delivery to the brain. This requires a multifaceted approach, incorporating advanced monitoring techniques, precise diagnostic methods, and targeted therapeutic interventions.
Key Points
- ICP monitoring is crucial for early detection of elevated ICP and prompt intervention
- CPP is a critical parameter in determining cerebral perfusion and oxygenation
- Targeted therapeutic interventions, such as CSF drainage and pharmacological agents, can effectively manage elevated ICP
- Advanced imaging modalities, including CT and MRI, are essential for diagnosing underlying causes of elevated ICP
- Neuroprotective strategies, such as hypothermia and sedation, can help mitigate secondary brain injury
Monitoring and Diagnosis of Elevated ICP
Accurate monitoring of ICP is essential for early detection of elevated ICP and prompt intervention. Various monitoring techniques are available, including invasive (e.g., intraventricular catheters, subarachnoid bolts) and non-invasive (e.g., transcranial Doppler, optic nerve sheath diameter) methods. Each technique has its advantages and limitations, and the choice of monitoring modality depends on the individual patient’s clinical context and underlying condition. Advanced imaging modalities, such as computed tomography (CT) and magnetic resonance imaging (MRI), are also critical for diagnosing the underlying cause of elevated ICP and guiding therapeutic interventions.
| Monitoring Modality | Description | Advantages | Limitations |
|---|---|---|---|
| Intraventricular Catheter | Direct measurement of ICP via a catheter inserted into the lateral ventricle | High accuracy, allows for CSF drainage | Invasive, risk of infection and hemorrhage |
| Subarachnoid Bolt | Measurement of ICP via a sensor inserted into the subarachnoid space | Less invasive than intraventricular catheter, relatively low risk of complications | Lower accuracy compared to intraventricular catheter, limited by presence of blood or debris |
| Transcranial Doppler | Non-invasive measurement of blood flow velocity in cerebral arteries | Non-invasive, relatively low cost, can be used for continuous monitoring | Lower accuracy compared to invasive methods, limited by operator expertise and patient cooperation |
Treatment and Management of Elevated ICP
Targeted therapeutic interventions are critical for managing elevated ICP and maintaining optimal CPP. These interventions can be broadly categorized into first-tier (e.g., CSF drainage, sedation, and analgesia) and second-tier (e.g., pharmacological agents, hypothermia, and decompressive craniectomy) therapies. The primary goal of these interventions is to reduce ICP, improve CPP, and mitigate secondary brain injury. Advanced imaging modalities, such as CT and MRI, are essential for diagnosing the underlying cause of elevated ICP and guiding therapeutic interventions.
First-Tier Therapies for Elevated ICP
First-tier therapies are initial interventions aimed at reducing ICP and improving CPP. These therapies include CSF drainage, sedation, and analgesia. CSF drainage is a highly effective method for reducing ICP, particularly in patients with hydrocephalus or other conditions characterized by impaired CSF absorption. Sedation and analgesia are also critical for managing agitation, pain, and discomfort, which can exacerbate elevated ICP.
Second-Tier Therapies for Elevated ICP
Second-tier therapies are reserved for patients who fail to respond to first-tier interventions or have severe elevated ICP. These therapies include pharmacological agents, such as mannitol and hypertonic saline, which can help reduce ICP by decreasing cerebral edema and improving cerebral perfusion. Hypothermia is also a valuable therapeutic strategy, as it can help reduce cerebral metabolism and mitigate secondary brain injury. Decompressive craniectomy is a surgical intervention that involves removing a portion of the skull to allow for expansion of the brain and reduction of ICP.
What are the most common causes of elevated ICP?
+The most common causes of elevated ICP include traumatic brain injury (TBI), stroke, intracranial hemorrhage, and tumors. Other causes include hydrocephalus, cerebral edema, and meningitis.
How is ICP monitored in clinical practice?
+ICP is monitored using various techniques, including invasive (e.g., intraventricular catheters, subarachnoid bolts) and non-invasive (e.g., transcranial Doppler, optic nerve sheath diameter) methods. The choice of monitoring modality depends on the individual patient's clinical context and underlying condition.
What are the primary goals of ICP medical management?
+The primary goals of ICP medical management are to maintain optimal cerebral perfusion pressure (CPP), ensure adequate oxygenation and nutrient delivery to the brain, and mitigate secondary brain injury. This requires a multifaceted approach, incorporating advanced monitoring techniques, precise diagnostic methods, and targeted therapeutic interventions.
In conclusion, ICP medical management is a complex and multifaceted field, requiring a comprehensive understanding of the physiological processes involved in maintaining optimal cerebral perfusion. By incorporating advanced monitoring techniques, precise diagnostic methods, and targeted therapeutic interventions, healthcare providers can effectively manage elevated ICP and improve patient outcomes. As a domain-specific expert, I emphasize the importance of individualized patient care, taking into account the unique clinical context and underlying condition of each patient. By adopting a nuanced and evidence-based approach to ICP management, we can optimize patient care and improve the lives of those affected by traumatic brain injury, stroke, and other neurological disorders.