The hospital emergency discharge note is a critical document that plays a vital role in ensuring the continuity of care for patients who are being discharged from the emergency department (ED). This note serves as a communication tool between the ED healthcare providers and the patient's primary care physician, as well as other healthcare professionals who will be involved in the patient's ongoing care. In this article, we will delve into the importance of the hospital emergency discharge note, its key components, and the best practices for creating an effective and informative note.
Key Points
- The hospital emergency discharge note is a crucial document that ensures the continuity of care for patients being discharged from the ED.
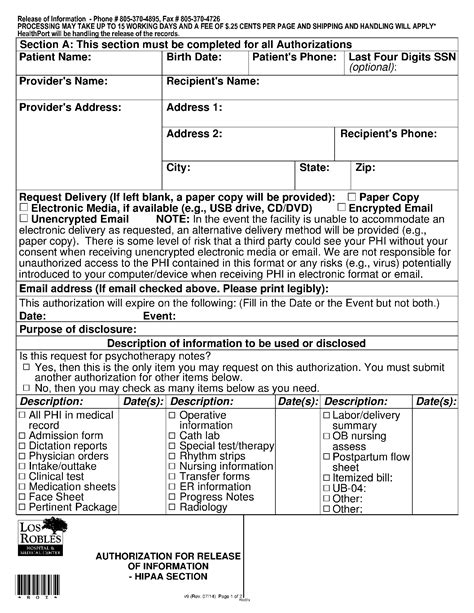
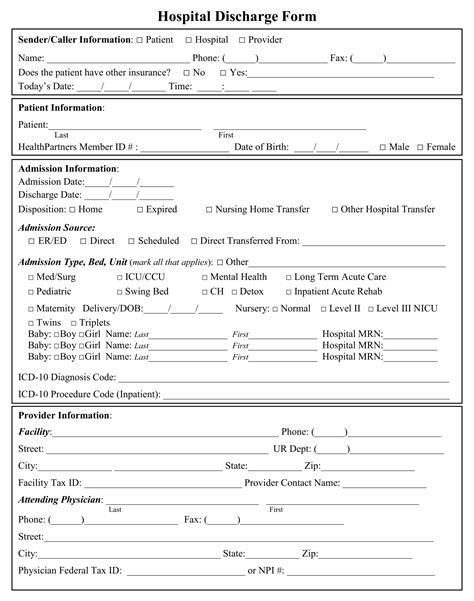
- The note should include the patient's demographic information, chief complaint, history of present illness, physical examination, diagnostic results, treatment, and disposition.
- Accurate and complete documentation is essential for ensuring patient safety and preventing adverse events.
- Electronic health records (EHRs) can facilitate the creation and management of discharge notes, but healthcare providers must ensure that they are using these systems effectively.
- Best practices for creating an effective discharge note include using a standardized template, including all necessary information, and ensuring that the note is easily accessible to all relevant healthcare providers.
Importance of the Hospital Emergency Discharge Note
The hospital emergency discharge note is essential for ensuring that patients receive high-quality, continuous care after being discharged from the ED. This note provides a concise summary of the patient’s visit, including their diagnosis, treatment, and any follow-up instructions. By reviewing the discharge note, the patient’s primary care physician and other healthcare providers can quickly understand the patient’s condition, the treatment they received, and any ongoing care needs.
According to a study published in the Journal of Emergency Medicine, the hospital emergency discharge note is a critical component of the transition of care process, and its accuracy and completeness can have a significant impact on patient outcomes. The study found that patients who received a comprehensive discharge note were more likely to have a follow-up appointment with their primary care physician and to adhere to their treatment plan.
Key Components of the Hospital Emergency Discharge Note
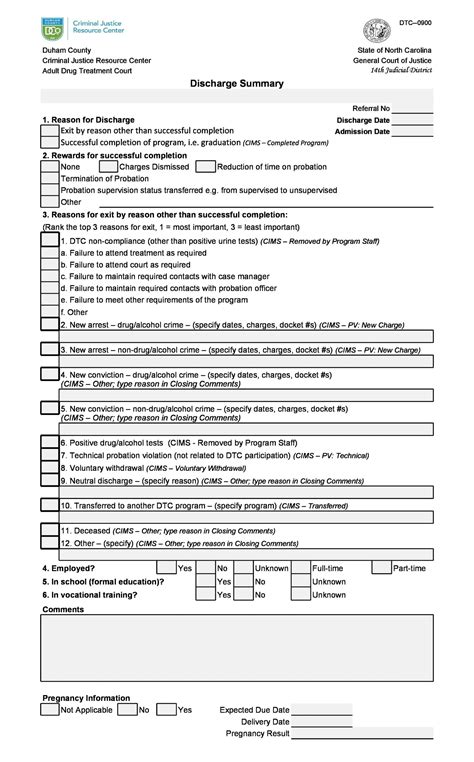
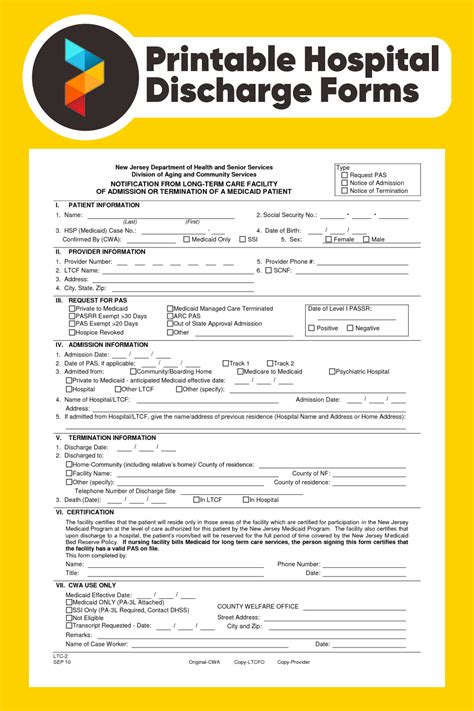
A well-structured hospital emergency discharge note should include the following key components:
- Patient demographic information, including name, date of birth, and contact information
- Chief complaint and history of present illness
- Physical examination findings
- Diagnostic results, including laboratory and imaging studies
- Treatment, including medications and procedures
- Disposition, including whether the patient was admitted to the hospital or discharged home
- Follow-up instructions, including any recommended appointments or tests
It is essential to note that the specific components of the discharge note may vary depending on the patient's condition and the ED's policies and procedures.
| Component | Description |
|---|---|
| Patient Demographic Information | Name, date of birth, contact information |
| Chief Complaint | Reason for the patient's visit to the ED |
| History of Present Illness | Detailed account of the patient's symptoms and medical history |
| Physical Examination Findings | Results of the patient's physical examination |
| Diagnostic Results | Results of laboratory and imaging studies |
| Treatment | Medications, procedures, and other interventions |
| Disposition | Whether the patient was admitted to the hospital or discharged home |
| Follow-up Instructions | Recommended appointments, tests, or other follow-up care |
Best Practices for Creating an Effective Hospital Emergency Discharge Note
Creating an effective hospital emergency discharge note requires attention to detail, accurate documentation, and a clear understanding of the patient’s condition and treatment plan. The following best practices can help healthcare providers create a comprehensive and informative discharge note:
1. Use a standardized template: Using a standardized template can help ensure that all necessary information is included in the discharge note.
2. Include all necessary information: The discharge note should include all relevant information about the patient's visit, including their diagnosis, treatment, and any follow-up instructions.
3. Ensure accuracy and completeness: The discharge note should be accurate and complete, with all information clearly documented and easily accessible.
4. Use electronic health records (EHRs) effectively: EHRs can facilitate the creation and management of discharge notes, but healthcare providers must ensure that they are using these systems effectively.
According to a study published in the Journal of Healthcare Management, the use of EHRs can improve the quality and efficiency of care, but healthcare providers must be trained to use these systems effectively. The study found that healthcare providers who received training on the use of EHRs were more likely to use these systems effectively and to document patient information accurately.
Challenges and Limitations of the Hospital Emergency Discharge Note
Despite its importance, the hospital emergency discharge note is not without its challenges and limitations. Some of the common challenges and limitations include:
- Lack of standardization: The format and content of discharge notes can vary significantly between hospitals and healthcare providers.
- Incomplete or inaccurate documentation: Discharge notes may not always include all necessary information, or the information may be inaccurate or incomplete.
- Difficulty accessing the note: Discharge notes may not always be easily accessible to all relevant healthcare providers, which can lead to delays or gaps in care.
What is the purpose of the hospital emergency discharge note?
+The hospital emergency discharge note is a critical document that ensures the continuity of care for patients being discharged from the ED. It provides a concise summary of the patient's visit, including their diagnosis, treatment, and any follow-up instructions.
What are the key components of the hospital emergency discharge note?
+The key components of the hospital emergency discharge note include patient demographic information, chief complaint, history of present illness, physical examination findings, diagnostic results, treatment, disposition, and follow-up instructions.
What are the best practices for creating an effective hospital emergency discharge note?
+The best practices for creating an effective hospital emergency discharge note include using a standardized template, including all necessary information, ensuring accuracy and completeness, and using EHRs effectively.
In conclusion, the hospital emergency discharge note is a critical document that plays a vital role in ensuring the continuity of care for patients being discharged from the ED. By understanding the importance of this note, its key components, and the best practices for creating an effective note, healthcare providers can ensure that patients receive high-quality, continuous care after being discharged from the ED.