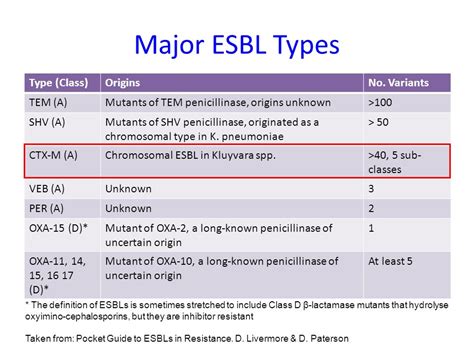
The abbreviation ESBL stands for Extended-Spectrum Beta-Lactamase, which refers to a type of enzyme produced by certain bacteria that confers resistance to a wide range of beta-lactam antibiotics, including penicillins, cephalosporins, and aztreonam. ESBL-producing bacteria are a significant concern in the medical field due to their ability to resist the effects of many commonly used antibiotics, making infections caused by these bacteria more challenging to treat.
Understanding ESBL-Producing Bacteria
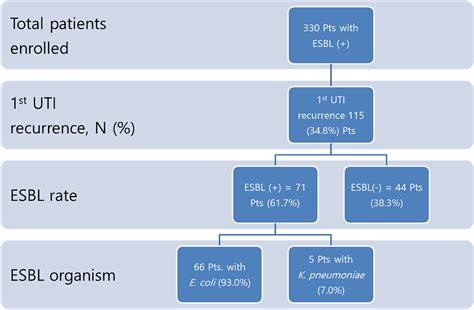
ESBL-producing bacteria are typically Gram-negative bacteria, such as Klebsiella pneumoniae and Escherichia coli (E. coli), that have acquired the ability to produce ESBL enzymes through genetic mutations or the acquisition of resistance genes from other bacteria. These enzymes work by breaking down the beta-lactam ring structure of antibiotics, rendering them ineffective against the bacteria.
Prevalence and Risk Factors
The prevalence of ESBL-producing bacteria varies globally, but they are increasingly being reported in healthcare settings, particularly in patients with weakened immune systems, those who have undergone invasive medical procedures, and individuals who have been exposed to broad-spectrum antibiotics. Risk factors for acquiring an ESBL-producing bacterial infection include recent hospitalization, residence in a long-term care facility, and travel to areas with high rates of antibiotic resistance.
| Common ESBL-Producing Bacteria | Associated Infections |
|---|---|
| Klebsiella pneumoniae | Urinary tract infections, pneumonia, bloodstream infections |
| Escherichia coli (E. coli) | Urinary tract infections, intra-abdominal infections, skin and soft tissue infections |
Clinical Implications and Management
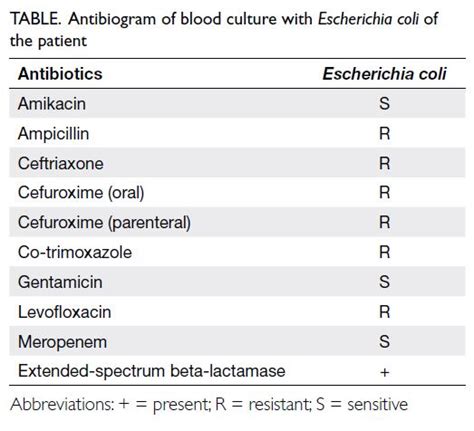
The clinical implications of ESBL-producing bacterial infections are significant, as they often require the use of broader-spectrum or more toxic antibiotics, which can lead to increased morbidity, mortality, and healthcare costs. Management strategies include the use of carbapenems, which are often considered the drugs of choice for treating serious infections caused by ESBL-producing bacteria, although resistance to these agents is also emerging.
Prevention and Control Measures
Prevention and control measures are crucial in mitigating the spread of ESBL-producing bacteria. These include hand hygiene, the use of personal protective equipment (PPE), and the implementation of contact precautions for patients known to be colonized or infected with ESBL-producing bacteria. Additionally, antimicrobial stewardship programs play a vital role in promoting the appropriate use of antibiotics, reducing the selective pressure that drives the development of resistance.
Key Points
- ESBL-producing bacteria are resistant to a wide range of beta-lactam antibiotics, complicating the treatment of infections.
- These bacteria are often associated with healthcare-associated infections and are more common in individuals with certain risk factors.
- Management involves the use of specific antibiotics and adherence to infection control practices.
- Prevention strategies include judicious antibiotic use, enhanced infection control measures, and the development of new antimicrobial agents.
- The emergence of ESBL-producing bacteria highlights the need for a multifaceted approach to combat antibiotic resistance.
In conclusion, ESBL-producing bacteria pose a significant challenge to public health due to their resistance to many commonly used antibiotics. Understanding the mechanisms of resistance, the risk factors for infection, and the clinical implications is essential for developing effective management and prevention strategies. By combining these approaches, healthcare professionals can work towards reducing the spread of these resistant bacteria and improving outcomes for patients infected with them.
What are ESBL-producing bacteria, and why are they a concern in medicine?
+ESBL-producing bacteria are a type of bacteria that have developed resistance to a wide range of beta-lactam antibiotics, making them challenging to treat. They are a concern because they can cause serious infections that are difficult to manage with standard antibiotic therapies.
How are ESBL-producing bacterial infections diagnosed?
+Diagnosis typically involves culturing the bacteria from a clinical specimen and performing antimicrobial susceptibility testing to determine the pattern of resistance. Molecular tests may also be used to detect the presence of ESBL genes.
What are the best practices for preventing the spread of ESBL-producing bacteria in healthcare settings?
+Best practices include strict adherence to hand hygiene, the use of personal protective equipment, contact precautions for colonized or infected patients, and the implementation of antimicrobial stewardship programs to promote the judicious use of antibiotics.