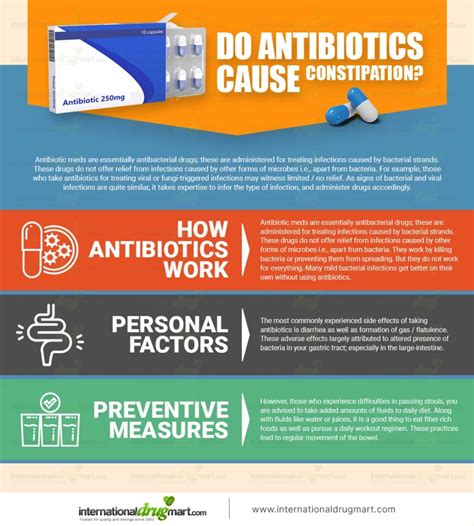
Antibiotics are a class of medications that have revolutionized the treatment of bacterial infections, saving countless lives and improving the quality of life for millions of people worldwide. However, like all medications, antibiotics can have unintended side effects, and one of the most common complaints is constipation. But do antibiotics really cause constipation, and if so, what are the underlying mechanisms and how can we manage this issue?
Key Points
- Antibiotics can alter the gut microbiome, leading to changes in bowel movements and potentially causing constipation.
- The likelihood of experiencing constipation as a side effect of antibiotics depends on various factors, including the type of antibiotic, dosage, and individual susceptibility.
- Certain antibiotics, such as those in the macrolide and fluoroquinolone classes, are more likely to cause constipation than others.
- Probiotics and prebiotics may help mitigate the risk of antibiotic-induced constipation by promoting a healthy balance of gut bacteria.
- Practicing good bowel habits, staying hydrated, and maintaining a balanced diet can also help alleviate constipation caused by antibiotics.
Understanding the Relationship Between Antibiotics and Constipation
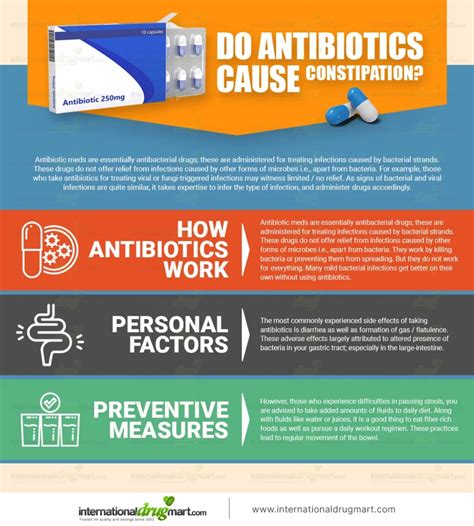
Constipation is a common side effect of many medications, including antibiotics. Studies have shown that up to 30% of patients taking antibiotics experience constipation, although the exact prevalence may vary depending on the specific antibiotic and population being studied. The relationship between antibiotics and constipation is complex and multifaceted, involving changes in the gut microbiome, alterations in bowel motility, and individual susceptibility factors.
The Role of the Gut Microbiome in Constipation
The gut microbiome plays a crucial role in maintaining healthy bowel function, including the regulation of bowel movements, the production of vitamins, and the metabolism of nutrients. Antibiotics can disrupt the delicate balance of the gut microbiome by killing off both pathogenic and beneficial bacteria, leading to changes in the composition and diversity of the microbial community. This dysbiosis can result in a range of symptoms, including constipation, diarrhea, and bloating.
| Antibiotic Class | Constipation Risk |
|---|---|
| Macrolides (e.g., erythromycin, clarithromycin) | Higher risk |
| Fluoroquinolones (e.g., ciprofloxacin, levofloxacin) | Higher risk |
| Cephalosporins (e.g., ceftriaxone, cefepime) | Lower risk |
| Penicillins (e.g., amoxicillin, penicillin) | Lower risk |

Managing Antibiotic-Induced Constipation
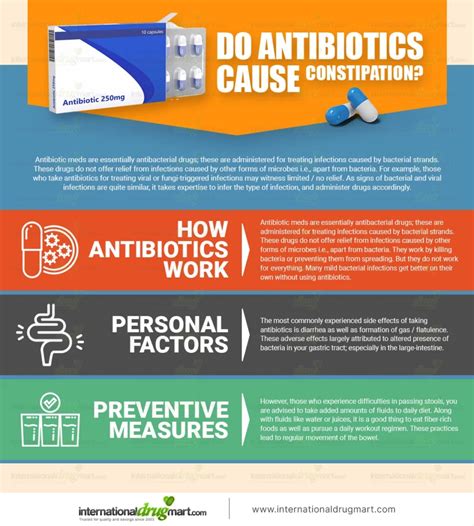
While antibiotics can increase the risk of constipation, there are several strategies that can help mitigate this side effect. Practicing good bowel habits, such as staying hydrated, exercising regularly, and maintaining a balanced diet rich in fiber, can help promote healthy bowel function. Additionally, probiotics and prebiotics may be beneficial in reducing the risk of antibiotic-induced constipation by promoting a healthy balance of gut bacteria.
Lifestyle Modifications for Preventing Constipation
Making simple lifestyle modifications can go a long way in preventing constipation when taking antibiotics. Staying hydrated by drinking plenty of water, exercising regularly, and avoiding foods that can exacerbate constipation, such as dairy products and processed foods, can help promote healthy bowel function. Furthermore, incorporating fermented foods, such as yogurt and kefir, into the diet can provide a natural source of probiotics and help maintain a healthy gut microbiome.
Can all antibiotics cause constipation?
+No, not all antibiotics are equally likely to cause constipation. The risk of constipation varies depending on the specific antibiotic, with some classes, such as macrolides and fluoroquinolones, being more commonly associated with this side effect.
How can I prevent constipation when taking antibiotics?
+To prevent constipation when taking antibiotics, it's essential to practice good bowel habits, such as staying hydrated, exercising regularly, and maintaining a balanced diet rich in fiber. Additionally, probiotics and prebiotics may be beneficial in reducing the risk of antibiotic-induced constipation.
Can probiotics help alleviate antibiotic-induced constipation?
+Yes, probiotics may be beneficial in alleviating antibiotic-induced constipation. By promoting a healthy balance of gut bacteria, probiotics can help regulate bowel function and reduce the risk of constipation.
In conclusion, while antibiotics can increase the risk of constipation, this side effect is not inevitable. By understanding the underlying mechanisms, recognizing individual susceptibility factors, and taking proactive steps to mitigate the risk of constipation, healthcare providers can help minimize the impact of antibiotics on bowel function and improve patient outcomes. As research continues to uncover the complex relationships between antibiotics, the gut microbiome, and bowel function, we can develop more effective strategies for managing antibiotic-induced constipation and promoting healthy bowel habits.