The conversion from Bumex (bumetanide) to Lasix (furosemide) is a common consideration in clinical practice, particularly in the management of edema and fluid overload in patients with heart failure, nephrotic syndrome, and other conditions. Bumetanide and furosemide are both loop diuretics, which work by inhibiting the sodium-potassium-chloride cotransporter in the ascending limb of the loop of Henle, leading to increased excretion of sodium, chloride, and water. Despite their similar mechanisms of action, the two drugs have different pharmacokinetic and pharmacodynamic profiles, necessitating careful consideration when converting from one to the other.
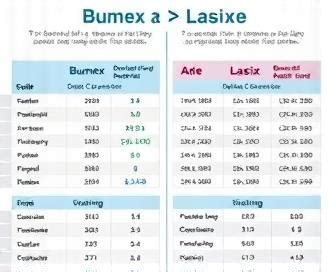
Bumetanide is approximately 40 times more potent than furosemide on a milligram-per-milligram basis. This significant difference in potency means that the dose of furosemide required to achieve the same diuretic effect as bumetanide is substantially higher. The generally recommended conversion ratio is 1 mg of bumetanide to 20-40 mg of furosemide, though this can vary depending on the patient's renal function, the specific clinical context, and the desired therapeutic effect. For example, in patients with normal renal function, a 1 mg dose of bumetanide might be equivalent to 20-25 mg of furosemide, while in those with impaired renal function, the equivalent dose of furosemide might need to be higher due to decreased drug efficacy.
Key Points
- Bumetanide is approximately 40 times more potent than furosemide.
- The conversion ratio from bumetanide to furosemide is generally 1:20 to 1:40.
- Renal function significantly affects the conversion and efficacy of both drugs.
- Close monitoring of patients during the conversion process is crucial to avoid dehydration and electrolyte imbalances.
- Individual patient factors, such as age, weight, and comorbid conditions, can influence the optimal conversion ratio.
Pharmacological Considerations
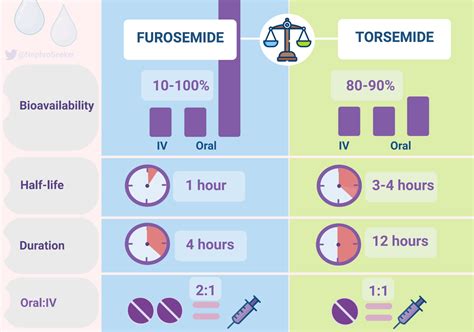
When converting from bumetanide to furosemide, it’s essential to consider the pharmacological profiles of both drugs. Bumetanide has a more rapid onset of action compared to furosemide, with peak effects observed within 30-60 minutes after oral administration. Furosemide, on the other hand, has a slightly slower onset of action, with peak diuretic effects typically occurring within 1-2 hours after oral administration. The duration of action for both drugs is approximately 4-6 hours, though this can vary based on renal function and the dose administered.
Clinical Implications
The clinical implications of converting from bumetanide to furosemide are significant and must be carefully managed to avoid adverse effects. One of the primary concerns is the risk of dehydration and electrolyte imbalances, particularly hypokalemia (low potassium levels), which can occur if the conversion results in excessive diuresis. Monitoring of serum electrolytes, including potassium, sodium, and chloride, as well as renal function, is crucial during this period. Additionally, patients should be instructed to report any signs of dehydration, such as excessive thirst, dark urine, or dizziness, promptly.
| Drug | Potency (Relative to Furosemide) | Onset of Action | Peak Effect | Duration of Action |
|---|---|---|---|---|
| Bumetanide | 40 times more potent | Rapid | 30-60 minutes | 4-6 hours |
| Furosemide | Reference | Slightly slower | 1-2 hours | 4-6 hours |
Renal Function Considerations
Renal function plays a critical role in the efficacy and safety of both bumetanide and furosemide. In patients with impaired renal function, the dose of furosemide may need to be increased to achieve the desired diuretic effect, as the drug’s efficacy decreases with declining renal function. Conversely, bumetanide may remain effective at lower doses even in the setting of renal impairment, though careful dose adjustment is still necessary to avoid toxicity. The estimation of glomerular filtration rate (GFR) can be a useful tool in guiding dose adjustments for both drugs in patients with renal impairment.
Practical Considerations for Conversion
In practice, the conversion from bumetanide to furosemide should be approached with caution, particularly in patients who are sensitive to changes in fluid status or electrolyte balance. A gradual conversion, with careful monitoring of the patient’s response, is often preferred. This may involve starting with a lower dose of furosemide than the calculated equivalent and adjusting upward as needed and as tolerated by the patient. Additionally, the use of combination therapy, where bumetanide and furosemide are used together, may be considered in certain clinical scenarios, though this requires careful consideration of the potential risks and benefits.
What is the primary consideration when converting from bumetanide to furosemide?
+The primary consideration is the significant difference in potency between the two drugs, with bumetanide being approximately 40 times more potent than furosemide, requiring careful dose adjustment to avoid adverse effects.
How does renal function affect the conversion from bumetanide to furosemide?
+Renal function significantly affects the conversion, as impaired renal function can decrease the efficacy of furosemide, potentially requiring higher doses, while bumetanide may remain effective at lower doses but still requires careful adjustment.
What are the key monitoring parameters during the conversion process?
+Key monitoring parameters include serum electrolytes (particularly potassium), renal function (through measures like GFR), and signs of dehydration or excessive diuresis, with close clinical observation for any adverse effects.
In conclusion, the conversion from bumetanide to furosemide requires a thorough understanding of the pharmacological profiles of both drugs, as well as careful consideration of individual patient factors, including renal function and sensitivity to diuretic effects. By approaching this conversion with caution, monitoring patients closely, and adjusting doses based on clinical response, healthcare providers can minimize the risks associated with this transition and optimize patient outcomes.