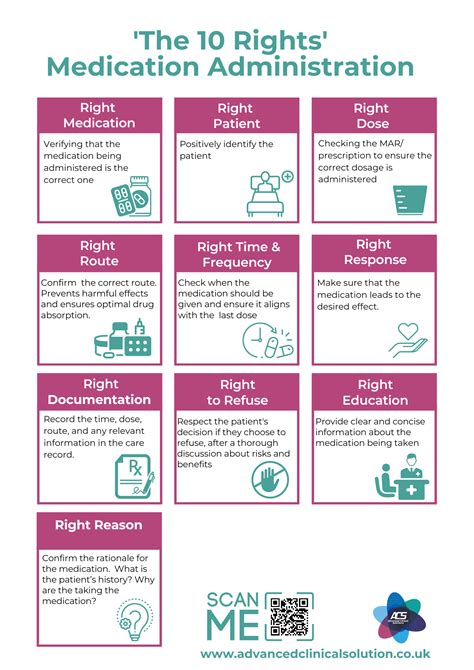
Medication administration is a critical aspect of healthcare, requiring precision and adherence to established protocols to ensure patient safety and optimal treatment outcomes. The 10 rights of medication administration serve as a foundational framework for healthcare professionals to follow, minimizing the risk of medication errors and promoting high-quality care. These rights are not merely guidelines but are grounded in evidence-based practice, reflecting the evolution of medication safety principles over the years.
Key Points
- The right patient: Ensuring medications are administered to the correct individual.
- The right medication: Selecting the appropriate medication for the patient's condition.
- The right dose: Administering the correct dosage to achieve therapeutic effects without causing harm.
- The right route: Using the appropriate method of administration for the medication.
- The right time: Administering medications at the scheduled time to maintain therapeutic levels.
- The right reason: Ensuring medications are given for the correct medical reason.
- The right response: Monitoring patients for the expected response to the medication.
- The right documentation: Accurately recording medication administration.
- The right to refuse: Respecting patients' rights to refuse medication.
- The right to education: Educating patients about their medications.
Introduction to the 10 Rights of Medication Administration
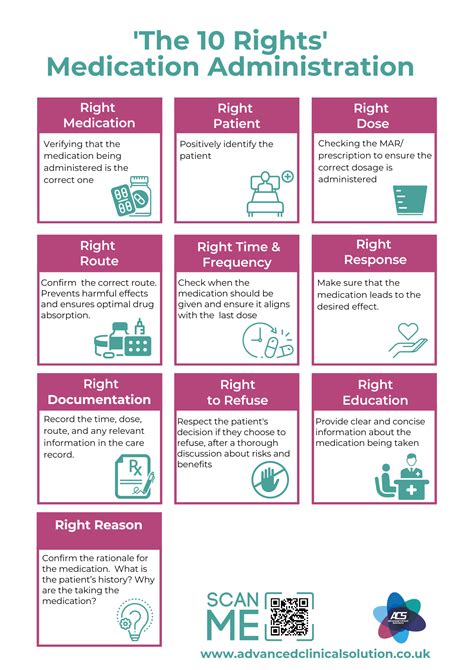
The concept of the 10 rights of medication administration has been a cornerstone of nursing and medical practice for decades, with its origins tracing back to the need for a systematic approach to medication safety. Initially, the focus was on the 5 rights (right patient, right drug, right dose, right route, and right time), but as the complexity of healthcare and the variety of medications increased, so did the need for a more comprehensive framework. The expansion to the 10 rights reflects a more holistic approach to medication administration, emphasizing not just the technical aspects but also the patient-centered and educational components of care.
The First Right: The Right Patient
Identifying the right patient is fundamental to safe medication administration. This involves verifying the patient’s identity using at least two identifiers, such as their name and date of birth, before administering any medication. Technology, such as barcode scanning, has significantly reduced errors in patient identification, making this process more efficient and reliable.
The Second Right: The Right Medication
Selecting the right medication is crucial for effective treatment and minimizing adverse effects. This involves not only choosing a medication that is appropriate for the patient’s condition but also considering factors such as potential drug interactions, allergies, and the patient’s medical history. The use of electronic health records (EHRs) and clinical decision support systems (CDSSs) has improved the ability to check for these factors at the point of ordering and administration.
The Third Right: The Right Dose
Administering the right dose is essential for achieving therapeutic effects while minimizing the risk of toxicity. Dosage calculations must be accurate, taking into account the patient’s weight, age, renal function, and other relevant factors. Automated systems for calculating doses and preparing medications have reduced the likelihood of human error in this critical step.
The Fourth Right: The Right Route
The route of administration is selected based on the medication’s formulation, the patient’s condition, and the desired onset of action. For example, intravenous administration is used for emergencies requiring rapid action, while oral medications are preferred for long-term management of chronic conditions. Understanding the pharmacokinetics of medications is essential for choosing the right route.
The Fifth Right: The Right Time
Administering medications at the right time ensures that therapeutic drug levels are maintained and that the medication’s effectiveness is optimized. This involves not only adhering to scheduled administration times but also considering factors such as the timing of meals, other medications, and sleep patterns, which can affect drug absorption and action.
The Sixth Right: The Right Reason
Medications should only be administered for a valid medical reason, as prescribed by a healthcare provider. This involves understanding the indication for the medication, potential side effects, and the expected outcome of treatment. Healthcare professionals must critically evaluate medication orders to ensure they are appropriate and necessary.
The Seventh Right: The Right Response
Monitoring for the right response to medication involves assessing whether the medication is achieving its intended effect and watching for potential adverse effects. This requires ongoing evaluation and adjustment of the treatment plan as necessary, based on patient feedback, clinical assessment, and laboratory data.
The Eighth Right: The Right Documentation
Accurate and timely documentation of medication administration is critical for ensuring continuity of care, facilitating communication among healthcare team members, and providing a legal record of treatment. Electronic medication administration records (eMARs) have improved the efficiency and accuracy of this process.
The Ninth Right: The Right to Refuse
Patient autonomy is a fundamental principle of healthcare, and patients have the right to refuse medications. Healthcare professionals must respect this right while also ensuring that patients are fully informed about the potential consequences of refusing treatment. This involves a sensitive and comprehensive discussion about the benefits and risks of the medication, as well as exploring alternative treatment options.
The Tenth Right: The Right to Education
Finally, patients have the right to be educated about their medications, including the name, purpose, dosage, potential side effects, and any necessary monitoring or follow-up. Patient education empowers individuals to take an active role in their care, improving adherence to medication regimens and overall health outcomes.
| Medication Administration Rights | Description |
|---|---|
| Right Patient | Verify patient identity before administration. |
| Right Medication | Choose the appropriate medication for the condition. |
| Right Dose | Calculate and administer the correct dose. |
| Right Route | Select the appropriate administration route. |
| Right Time | Administer medications at the scheduled time. |
| Right Reason | Ensure medications are given for a valid medical reason. |
| Right Response | Monitor for the expected response to the medication. |
| Right Documentation | Accurately record medication administration. |
| Right to Refuse | Respect patients' rights to refuse medication. |
| Right to Education | Educate patients about their medications. |

Implementing the 10 Rights in Practice
Implementation of the 10 rights requires a multifaceted approach, including education, policy development, and the adoption of technology to support safe medication practices. Healthcare institutions must foster a culture of safety, encouraging open communication and reporting of near misses or errors without fear of retribution. Continuous quality improvement initiatives should focus on identifying vulnerabilities in the medication administration process and implementing evidence-based solutions to address these gaps.
Role of Technology in Medication Safety
Technology plays a pivotal role in enhancing medication safety, from electronic prescribing systems that check for potential drug interactions and allergies, to automated dispensing cabinets that control access to medications and barcoding systems that verify the right patient, medication, dose, route, and time at the point of administration. These technologies not only reduce errors but also streamline workflows, allowing healthcare professionals to focus on patient care.
Challenges and Future Directions
Despite advancements in medication safety, challenges persist, including the complexity of medication regimens, the increasing burden of healthcare-associated costs, and the need for ongoing education and training of healthcare professionals. Future directions in medication administration will likely involve further integration of artificial intelligence and machine learning to predict and prevent errors, as well as a continued emphasis on patient-centered care and empowerment through education and involvement in the medication use process.
What is the primary goal of the 10 rights of medication administration?
+The primary goal is to ensure patient safety by minimizing medication errors through a systematic approach to medication administration.
How does technology support the implementation of the 10 rights?
+Technology supports the 10 rights through electronic health records, barcode scanning, automated dispensing systems, and clinical decision support systems, which help verify patient identity, check for drug interactions, and ensure accurate documentation.
Why is patient education considered one of the rights of medication administration?
+Patient education is crucial because it empowers patients to understand their medications, recognize potential side effects, and adhere to their medication regimens, ultimately improving health outcomes and safety.
In conclusion, the 10 rights of medication administration provide a comprehensive framework for ensuring the safe and effective use of medications. By understanding and applying these rights, healthcare professionals can significantly enhance patient safety and the quality of care provided. As healthcare continues to evolve, the importance of these principles will only continue to grow, serving as the foundation for innovative approaches to medication administration and patient care.